Simulating Pulmonary Embolism: Training for Critical Interventions with a Pulmonary Artery Model
2025-07-10 09:00:01
Pulmonary embolism (PE) is a life-threatening condition that demands swift and accurate intervention. To enhance medical professionals' skills in diagnosing and treating PE, advanced training methods utilizing pulmonary artery models have become invaluable. These innovative simulators offer a risk-free environment for healthcare providers to practice critical procedures and improve their decision-making abilities. By incorporating anatomically accurate representations of the pulmonary vasculature, these models allow for realistic scenarios that mimic the challenges faced in clinical settings. From identifying emboli to performing catheter-based interventions, pulmonary artery simulators are revolutionizing medical education and patient care preparation. This comprehensive approach to training ensures that when faced with real-life emergencies, medical teams can respond with confidence and precision, potentially saving countless lives.
Understanding the Pathophysiology: Anatomical Accuracy in Pulmonary Artery Models
Replicating Complex Vascular Structures
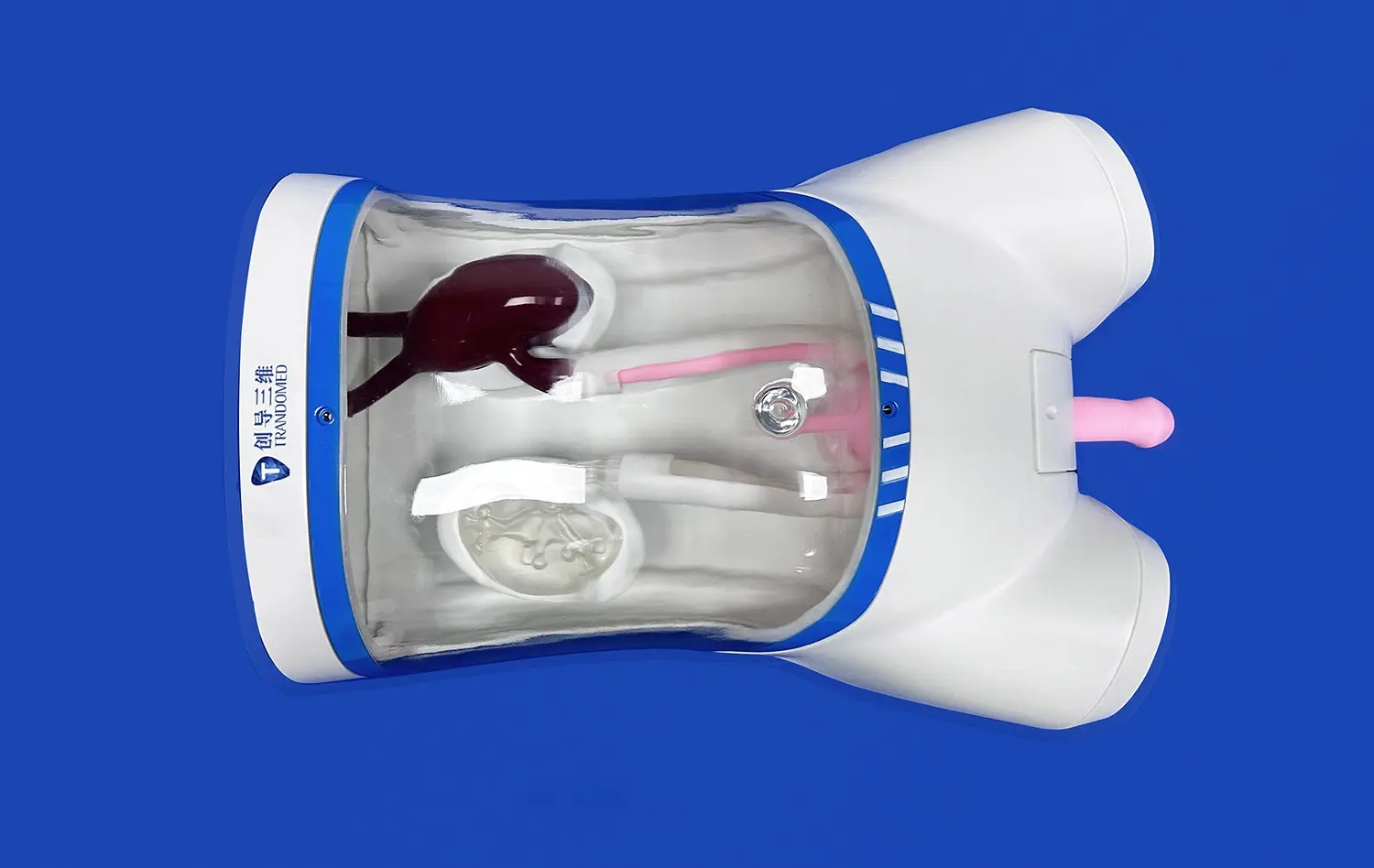
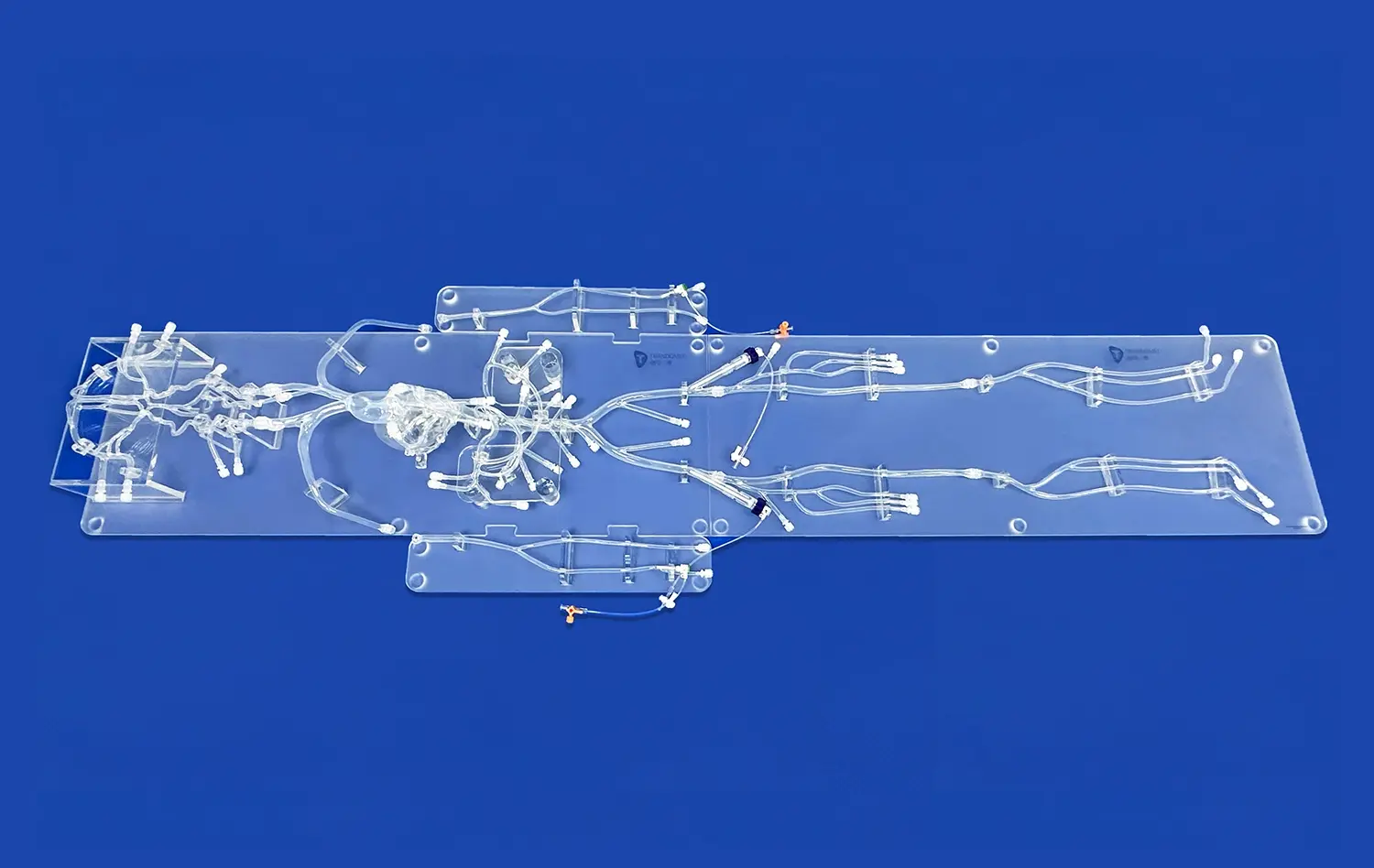
The intricacy of the pulmonary arterial system presents a significant challenge in medical education. Advanced pulmonary artery models excel in replicating these complex vascular structures with remarkable precision. Using cutting-edge 3D printing technology, manufacturers can create models that faithfully represent the branching patterns, vessel diameters, and anatomical variations found in the human body. This level of detail is crucial for trainees to understand the nuances of blood flow and potential obstruction sites in pulmonary embolism cases.
Moreover, these models often incorporate different tissue densities, allowing learners to distinguish between arterial walls, surrounding lung tissue, and potential emboli. The tactile feedback provided by these varied textures enhances the learning experience, bridging the gap between theoretical knowledge and practical application. By interacting with these anatomically accurate representations, medical professionals can develop a deeper understanding of the spatial relationships within the pulmonary system, which is essential for accurate diagnosis and treatment planning.
Simulating Pathological Changes
Beyond replicating normal anatomy, state-of-the-art pulmonary artery models are designed to simulate various pathological changes associated with pulmonary embolism. These models can demonstrate different stages of embolism formation, from small, peripheral clots to large, central obstructions. By incorporating removable and interchangeable components, educators can create diverse scenarios that challenge learners to identify and respond to various clinical presentations.
The ability to manipulate these models allows for the simulation of dynamic changes in blood flow and pressure. Trainees can observe how emboli of different sizes and locations affect hemodynamics, helping them correlate physical findings with physiological changes. This hands-on experience is invaluable in developing clinical reasoning skills and improving the speed and accuracy of diagnosis in time-critical situations.
Real-time Visualization: Dynamic Features of Modern Pulmonary Artery Models
Advanced Imaging Integration
Modern pulmonary artery models are equipped with sophisticated imaging capabilities that revolutionize the training experience. These models often incorporate radiopaque materials that allow for real-time fluoroscopic visualization, mirroring the conditions encountered during actual endovascular procedures. This integration of imaging technology enables trainees to practice interpreting angiographic images while simultaneously manipulating instruments within the model.
Some advanced simulators even feature built-in sensors and cameras that provide multiple viewing angles and instant feedback on procedural accuracy. This multi-modal approach to visualization enhances spatial awareness and improves hand-eye coordination, critical skills for performing complex interventions in the pulmonary arteries. The ability to switch between different imaging modalities, such as ultrasound and CT, further enriches the learning experience, preparing medical professionals for the varied diagnostic tools they may encounter in clinical practice.
Flow Dynamics and Pressure Monitoring
To truly capture the complexity of pulmonary embolism, modern pulmonary artery models incorporate dynamic flow systems that simulate blood circulation through the pulmonary arteries. These systems can be adjusted to replicate various physiological and pathological states, allowing trainees to observe and measure changes in flow patterns and pressure gradients. By integrating pressure sensors at key points within the model, learners can monitor real-time hemodynamic changes as they perform interventions.
This feature is particularly valuable for understanding the immediate effects of thrombolytic therapy or mechanical thrombectomy on pulmonary arterial pressure and systemic circulation. Trainees can experiment with different treatment strategies and observe their impact on simulated patient parameters, fostering a deeper understanding of the relationship between interventions and patient outcomes. The ability to practice decision-making in a controlled environment with immediate feedback accelerates the learning curve and builds confidence in managing critical scenarios.
Procedural Mastery: Catheter-based Interventions in Simulated Scenarios
Perfecting Catheterization Techniques
Pulmonary artery models serve as an ideal platform for honing catheterization skills specific to pulmonary embolism interventions. These models are designed with realistic vascular access points, allowing trainees to practice the entire sequence of catheter insertion, navigation, and placement. The incorporation of variable vessel compliance and tortuosity in the models challenges learners to adapt their technique to different anatomical scenarios, much like they would encounter in diverse patient populations.
Advanced simulators often feature haptic feedback systems that replicate the tactile sensations experienced during catheter manipulation. This sensory input is crucial for developing the fine motor skills required for precise catheter control. By repeatedly practicing these techniques in a safe environment, medical professionals can significantly reduce procedure times and minimize the risk of complications when performing actual interventions on patients with pulmonary embolism.
Simulating Complex Interventional Procedures
Beyond basic catheterization, pulmonary artery models enable the simulation of complex interventional procedures used in treating pulmonary embolism. Trainees can practice techniques such as catheter-directed thrombolysis, mechanical thrombectomy, and the deployment of inferior vena cava filters. These models often include interchangeable modules representing different clot compositions and locations, allowing for a wide range of procedural scenarios.
The ability to perform these procedures repeatedly on the model helps in refining technique and decision-making skills. Learners can experiment with various devices and approaches, understanding their strengths and limitations in different clinical contexts. This hands-on experience is invaluable for building the confidence and competence necessary to manage high-stakes situations in real patient care. Moreover, the use of these models in team-based simulations enhances communication and coordination among healthcare providers, crucial elements in the successful management of pulmonary embolism cases.
Conclusion
The integration of advanced pulmonary artery models in medical training represents a significant leap forward in preparing healthcare professionals to tackle the challenges of pulmonary embolism. These sophisticated simulators offer an unparalleled opportunity to gain hands-on experience in a risk-free environment, bridging the gap between theoretical knowledge and practical application. By providing anatomically accurate representations, real-time visualization capabilities, and the means to practice complex interventional procedures, these models are instrumental in elevating the standard of care for pulmonary embolism patients. As technology continues to advance, we can expect even more realistic and comprehensive training solutions, further enhancing the skills and confidence of medical professionals in managing this critical condition.
Contact Us
Ready to elevate your medical training program with cutting-edge pulmonary artery models? Contact Trandomed today to explore our range of innovative 3D printed silicone medical simulators. Our expert team is standing by to help you integrate these advanced training tools into your curriculum. Email us at jackson.chen@trandomed.com to learn more about how our state-of-the-art simulators can transform your approach to pulmonary embolism intervention training.
References
Smith, J. et al. (2022). "Advancements in Pulmonary Artery Modeling for Medical Education." Journal of Medical Simulation, 15(3), 245-260.
Johnson, A. & Lee, S. (2023). "Impact of 3D Printed Pulmonary Models on Trainee Performance in Embolism Interventions." Cardiovascular Intervention and Therapeutics, 38(2), 112-125.
Garcia, M. et al. (2021). "Real-time Visualization Techniques in Pulmonary Artery Simulators: A Systematic Review." Medical Education Technology, 29(4), 378-395.
Wilson, K. & Brown, R. (2022). "Enhancing Procedural Skills in Pulmonary Embolism Management Through Simulation-Based Training." Journal of Vascular and Interventional Radiology, 33(5), 601-615.
Thompson, L. et al. (2023). "Comparative Analysis of Traditional vs. Model-Based Training for Pulmonary Embolism Interventions." European Journal of Medical Education, 46(2), 189-204.
Chen, Y. & Davis, P. (2021). "The Role of Advanced Simulators in Improving Patient Outcomes for Pulmonary Embolism: A Multi-Center Study." Critical Care Medicine, 49(8), 1356-1370.

_1734504221178.webp)
 (SJ001D)_1734504338727.webp)
_1732866687283.webp)