How Are Aneurysm Models Used in Postgraduate Neurosurgical Courses?
Realistic Simulation for Procedural Training
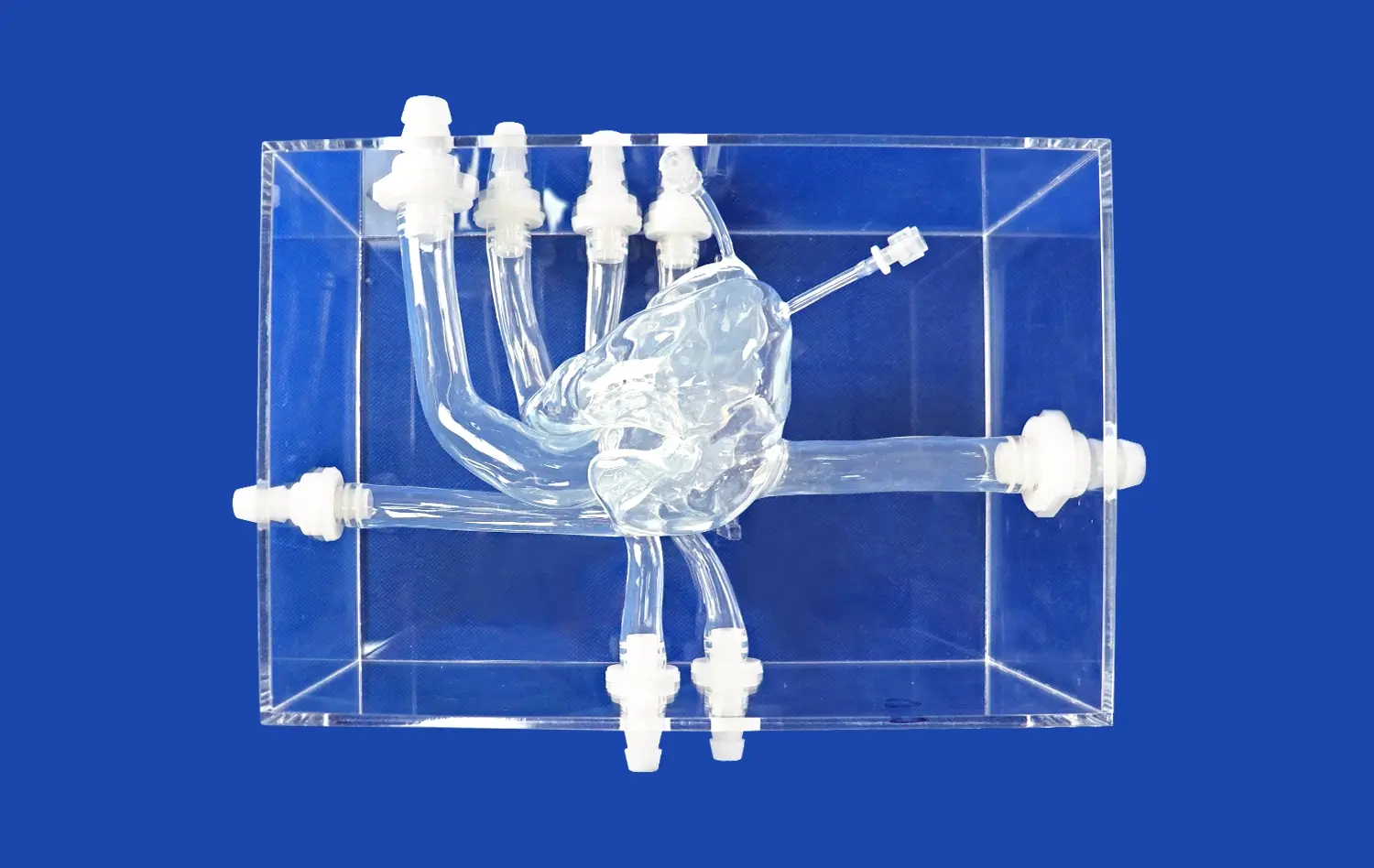
Aneurysm models, such as the Intracranial Vascular with Aneurysm Model (SJX011), offer an unparalleled platform for procedural training in postgraduate neurosurgical courses. These models meticulously replicate the complex anatomy of cerebral vasculature, including the anterior cerebral artery (ACA), middle cerebral artery (MCA), and the tortuous internal carotid artery. The inclusion of multiple aneurysms at various locations allows trainees to practice a wide range of interventions, from endovascular coiling to microsurgical clipping.
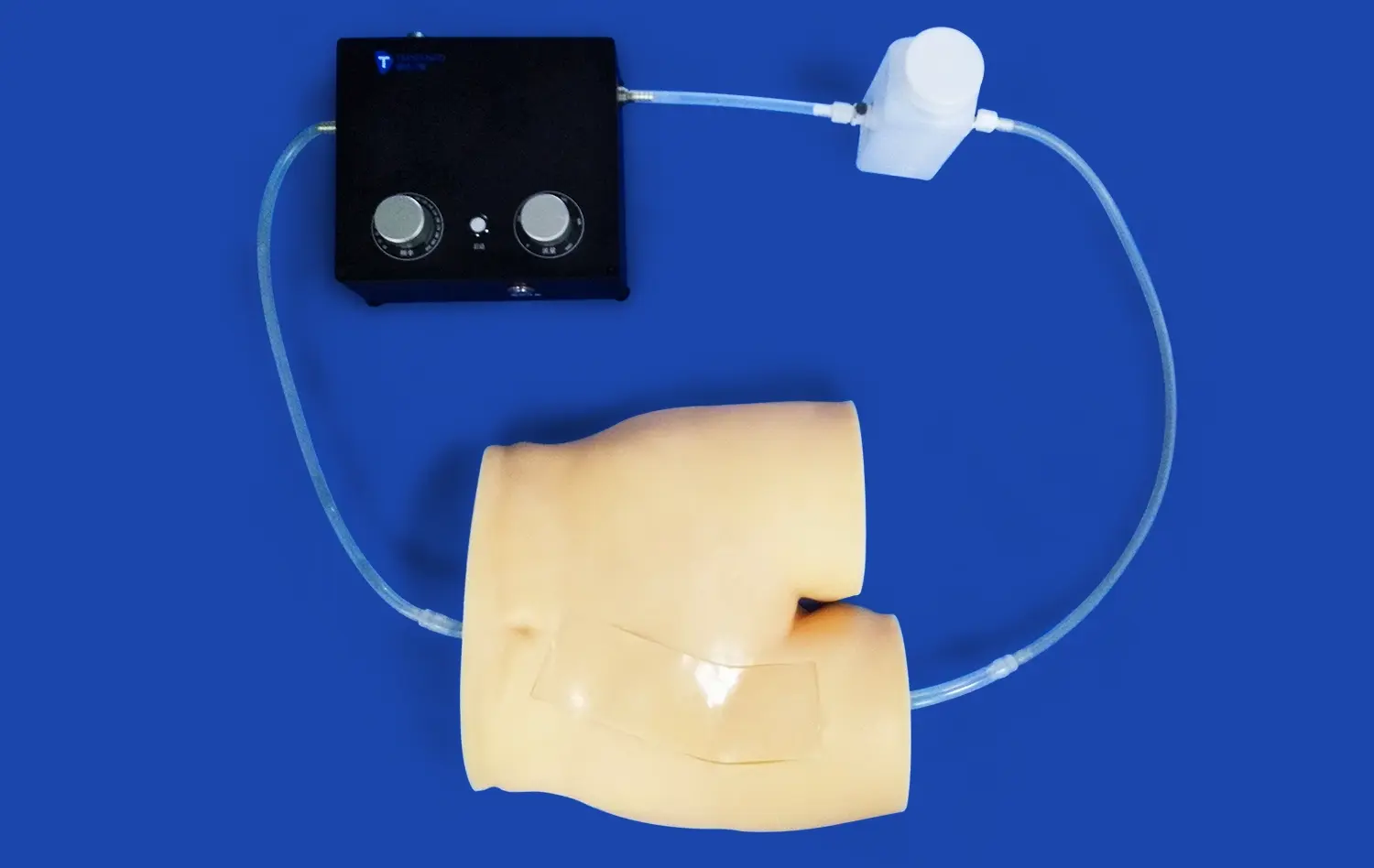
The tactile feedback and visual fidelity provided by these models enable neurosurgical residents to develop the fine motor skills and spatial awareness necessary for delicate procedures. By working with these lifelike representations, trainees can rehearse critical steps of aneurysm treatment, such as navigating through tortuous vessels, selecting appropriate instruments, and executing precise maneuvers without the pressure of operating on actual patients.
Case-Based Learning and Problem-Solving
Aneurysm models serve as excellent tools for case-based learning in postgraduate neurosurgical education. Instructors can create diverse scenarios by altering the number, size, and location of aneurysms on the models. This versatility allows for the simulation of rare or complex cases that trainees might not encounter frequently in clinical practice but need to be prepared for.
Through these simulated cases, postgraduate students engage in critical thinking and problem-solving exercises. They learn to assess the risks and benefits of different treatment approaches, consider patient-specific factors, and make informed decisions about the most appropriate intervention strategy. This process helps develop clinical reasoning skills that are essential for successful neurosurgical practice.
Objective Assessment and Skill Evaluation
Aneurysm models provide an objective means of assessing and evaluating the skills of neurosurgical trainees. Course instructors can use these models to create standardized tests that measure a trainee's proficiency in various aspects of aneurysm treatment. Metrics such as procedure time, accuracy of aneurysm occlusion, and preservation of parent vessels can be quantified and compared against established benchmarks.
This objective assessment allows for tracking individual progress over time and identifying areas that require further improvement. It also enables program directors to ensure that all trainees meet the necessary competency levels before advancing to more complex procedures or graduating from their postgraduate training.
Structured Learning Pathways with Anatomical Simulation Models
Progressive Skill Development
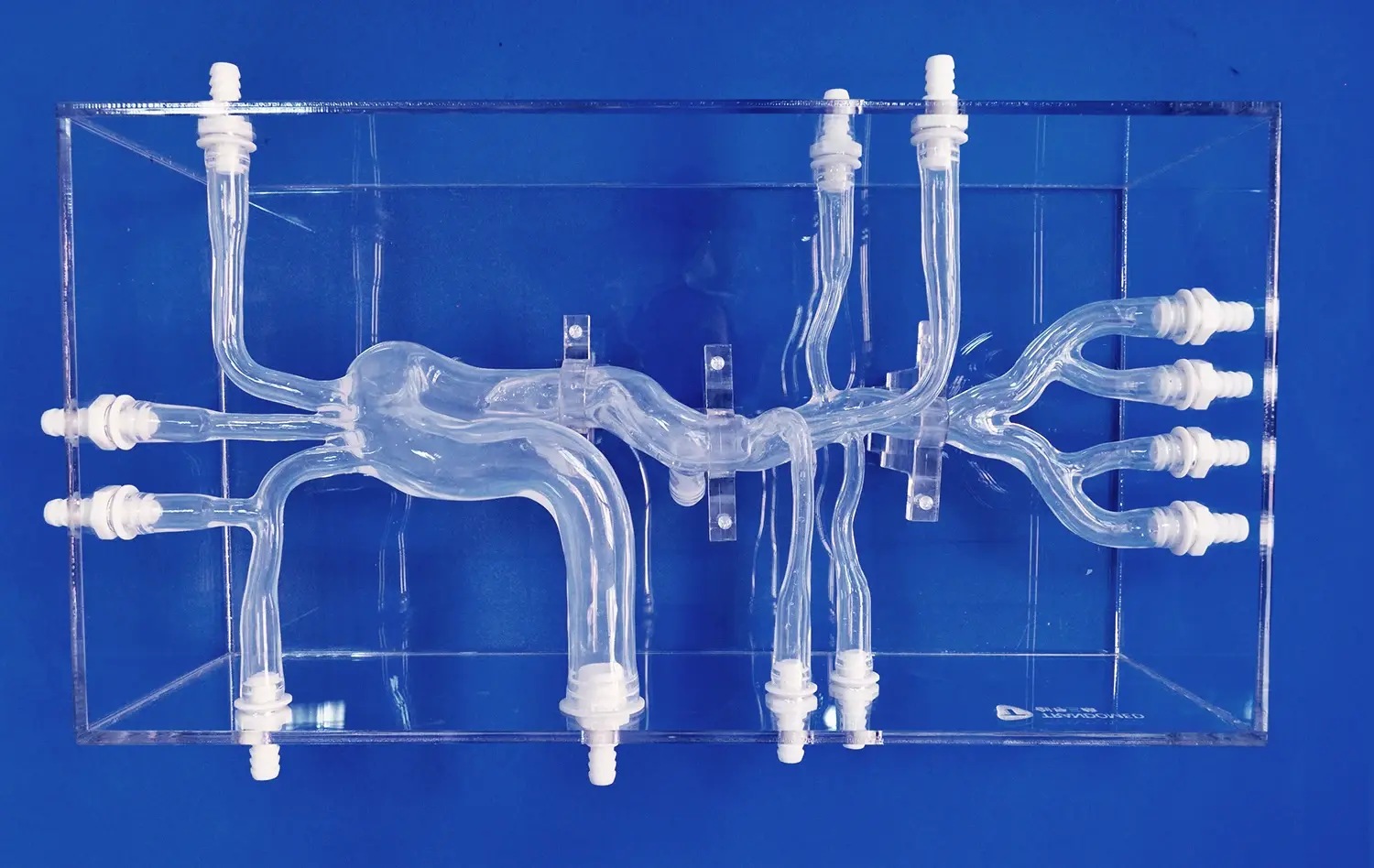
Structured learning pathways incorporating anatomical simulation models, particularly aneurysm models, offer a systematic approach to skill development in neurosurgical education. These pathways typically begin with basic familiarization of cerebral vascular anatomy using simplified models. As trainees progress, they encounter increasingly complex aneurysm scenarios that challenge their growing skillset.
For instance, a learning pathway might start with practicing basic catheterization techniques on straightforward vessel models. It then advances to navigating through more tortuous vasculature, such as the internal carotid artery with its characteristic bends. Finally, trainees would tackle complex aneurysm configurations, like those found at arterial bifurcations or in hard-to-reach locations.
This graduated approach ensures that learners build a solid foundation of skills and confidence before attempting more challenging procedures. It also allows for the integration of various treatment modalities, from endovascular techniques to open surgical approaches, providing a comprehensive neurosurgical education.
Multimodal Learning Integration
Aneurysm models serve as a focal point for integrating various learning modalities in neurosurgical education. While hands-on practice with the models is crucial, it is most effective when combined with other educational resources and techniques. For example, trainees might begin by studying detailed 3D renderings of aneurysm anatomy, followed by watching video demonstrations of expert surgeons performing procedures on similar models.
Virtual reality simulations can complement physical aneurysm models, allowing trainees to practice in a fully immersive environment before applying their skills to tangible models. This multimodal approach caters to different learning styles and reinforces knowledge through repetition across various platforms.
Additionally, group discussions and case presentations centered around aneurysm models encourage peer-to-peer learning and the exchange of ideas. This collaborative environment mimics the multidisciplinary approach often required in complex neurovascular cases.
Customized Learning Experiences
One of the significant advantages of using aneurysm models in structured learning pathways is the ability to customize the educational experience. Advanced manufacturing techniques, such as those employed by Trandomed, allow for the creation of patient-specific models based on actual clinical data. This customization enables educators to tailor learning experiences to the specific needs of individual trainees or to focus on particular types of aneurysms that are challenging to treat.
For instance, if a trainee shows particular difficulty with a certain type of aneurysm or surgical approach, additional models can be created to provide targeted practice. Similarly, if a neurosurgical program wants to emphasize a new treatment technique, custom models can be designed to facilitate its integration into the curriculum.
This level of customization ensures that the learning pathway remains relevant and adaptable to the evolving field of neurosurgery, as well as to the individual progress of each trainee.
Curriculum Integration for Specialized Aneurysm Treatment Techniques
Endovascular Technique Training
Integrating aneurysm models into the curriculum for specialized endovascular techniques has revolutionized training in this rapidly evolving field. Models like the SJX011 provide an ideal platform for practicing catheter navigation through complex vascular anatomy. Trainees can hone their skills in accessing aneurysms located in challenging positions, such as those arising from the tortuous segments of the internal carotid artery.
The curriculum typically includes progressive training stages, beginning with basic wire and catheter manipulation. As trainees advance, they practice more complex techniques such as balloon-assisted coiling, stent-assisted coiling, and flow diversion. The ability to work with replaceable aneurysm lesions on these models allows for repeated practice and experimentation with various endovascular devices and approaches.
Moreover, the integration of angiographic imaging simulation with physical aneurysm models enhances the realism of endovascular training. This combined approach helps trainees develop the hand-eye coordination and spatial awareness needed for fluoroscopy-guided procedures.
Microsurgical Clipping Techniques
For neurosurgical programs focusing on open surgical techniques, aneurysm models play a crucial role in teaching microsurgical clipping. The curriculum integration in this area emphasizes the development of fine motor skills and spatial awareness required for successful aneurysm obliteration.
Trainees begin by practicing basic microsurgical techniques such as vessel dissection and clip application on simple aneurysm configurations. As they progress, they encounter more challenging scenarios, including wide-necked aneurysms, multiple aneurysms, and those in deep-seated locations. The use of models with varying degrees of vessel wall elasticity and aneurysm dome fragility adds another layer of realism to the training experience.
The curriculum also incorporates exercises in selecting appropriate clip types and sizes, as well as techniques for temporary vessel occlusion and intraoperative aneurysm rupture management. By integrating aneurysm models into regular skills lab sessions, programs ensure that trainees maintain and continuously improve their microsurgical abilities throughout their education.
Hybrid and Emerging Treatment Approaches
As neurovascular treatment continues to evolve, aneurysm models are proving invaluable in curriculum integration for hybrid and emerging techniques. These models provide a platform for exploring innovative approaches that combine endovascular and open surgical methods, such as bypass procedures followed by parent vessel occlusion.
The curriculum for these advanced techniques often involves interdisciplinary collaboration, bringing together experts in neurosurgery, interventional neuroradiology, and biomedical engineering. Trainees work with specially designed models that allow for both endovascular access and simulated craniotomy, enabling them to practice complex, multi-stage procedures.
Furthermore, aneurysm models are instrumental in introducing trainees to cutting-edge technologies like robotics-assisted neurosurgery and augmented reality surgical navigation. By incorporating these models into the curriculum, neurosurgical programs ensure that their graduates are prepared to adopt and contribute to the future of aneurysm treatment.
Conclusion
The integration of aneurysm models into advanced neurosurgical education has transformed the landscape of training and skill development in this critical field. These sophisticated simulation tools provide an unparalleled platform for hands-on learning, allowing trainees to master complex procedures in a risk-free environment. From structured learning pathways to specialized curriculum integration, aneurysm models have proven to be versatile and indispensable assets in neurosurgical education. As the field continues to advance, these models will undoubtedly play an increasingly pivotal role in shaping the next generation of skilled neurosurgeons, ultimately contributing to enhanced patient care and improved outcomes in the treatment of cerebral aneurysms.
Contact Us
For more information on how Trandomed's state-of-the-art aneurysm models can elevate your neurosurgical training program, please contact us at jackson.chen@trandomed.com. Discover how our customizable solutions can meet your specific educational needs and help you stay at the forefront of neurosurgical innovation.
_1735798438356.webp)