How Do Models Facilitate Preclinical Testing of New Devices?
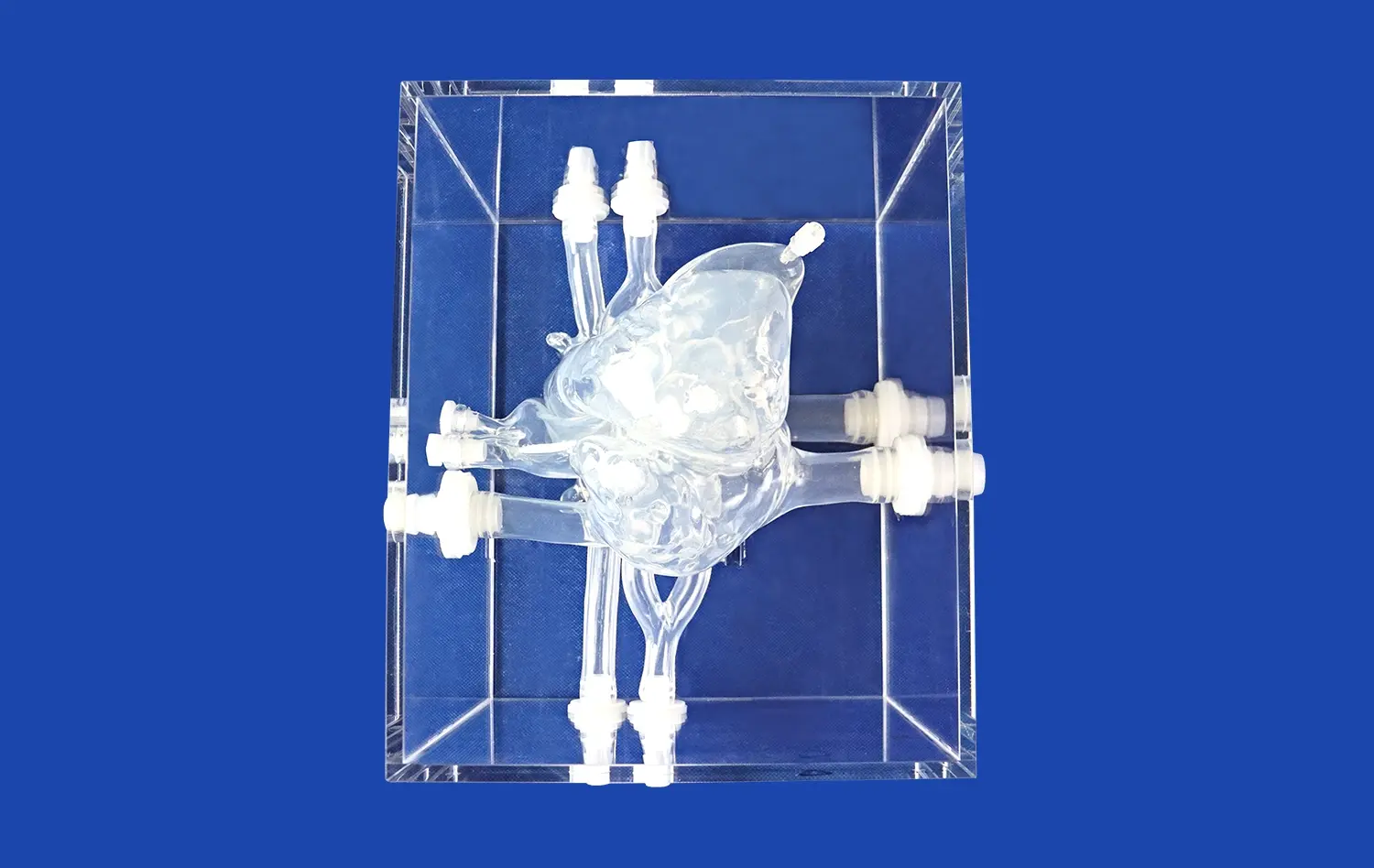
Aortic dissection models serve as indispensable tools in the preclinical testing phase of new medical devices. These sophisticated simulations offer a range of benefits that contribute to the development and refinement of cutting-edge interventional technologies.
Anatomical Accuracy for Realistic Testing
One of the primary advantages of using aortic dissection models in device development is their anatomical accuracy. These models, crafted using advanced 3D printing techniques and based on real patient data, provide a highly realistic representation of the aorta and its surrounding structures. This level of detail allows researchers to assess how new devices interact with the complex geometry of the aortic arch, descending aorta, and branching vessels.
The anatomical precision of these models enables developers to evaluate crucial factors such as:
- Device navigation through tortuous vessels
- Deployment accuracy in specific aortic segments
- Potential interactions with adjacent anatomical structures
By simulating these conditions, researchers can identify and address potential challenges before progressing to animal studies or human trials, significantly reducing risks and optimizing device design.
Pathological Replication for Targeted Solutions
Aortic dissection models excel in replicating the pathological features of this complex cardiovascular condition. The ability to incorporate specific dissection patterns, such as Stanford Type A or Type B dissections, allows developers to tailor their devices to address particular clinical scenarios.
Key pathological features that can be simulated include:
- Intimal tears and false lumen formation
- Varying degrees of luminal obstruction
- Compromised blood flow to vital organs
This pathological accuracy enables researchers to assess how their devices perform in managing the unique challenges posed by aortic dissections, such as sealing entry tears, restoring true lumen patency, or preserving blood flow to critical branch vessels.
Reproducibility for Comparative Analysis
The use of standardized aortic dissection models in preclinical testing offers a significant advantage in terms of reproducibility. Unlike biological specimens, which can vary considerably between individuals, these synthetic models provide a consistent testing environment across multiple experiments.
This reproducibility is crucial for:
- Comparing different device iterations
- Evaluating various deployment techniques
- Assessing the performance of competing technologies
By eliminating variables associated with biological variation, researchers can focus on the specific attributes of their devices, leading to more reliable and meaningful test results. This approach streamlines the development process and facilitates data-driven decision-making in device refinement.
Simulation-Based Evaluation of Stents and Grafts
Aortic dissection models play a crucial role in the evaluation of stents and grafts, two primary interventional devices used in treating this complex cardiovascular condition. These simulations provide a controlled environment for assessing various aspects of stent and graft performance, contributing to the development of more effective and safer treatment options.
Deployment Accuracy and Conformability
One of the key aspects of stent and graft evaluation using aortic dissection models is assessing deployment accuracy and conformability. These models allow researchers to simulate the precise placement of devices within the aorta, mimicking real-world clinical scenarios.
Factors that can be evaluated include:
- Ease of navigation through the vascular system
- Accuracy of deployment at the target site
- Conformability to the aortic wall curvature
By using models with varying aortic arch configurations, such as type I, type II, or type III arches, developers can optimize their devices to accommodate different anatomical variations. This approach helps in creating stents and grafts that can be more universally applied across diverse patient populations.
Sealing and Exclusion of False Lumen
Aortic dissection models are particularly valuable in evaluating the sealing capabilities of stents and grafts. The ability to exclude the false lumen and promote thrombosis is crucial for successful treatment outcomes.
Simulations allow researchers to assess:
- Effectiveness of proximal and distal seal zones
- Potential for endoleaks or persistent false lumen perfusion
- Impact on branch vessel perfusion
By incorporating features such as multiple entry tears or complex dissection flaps, these models challenge the sealing performance of devices under various pathological conditions. This rigorous testing helps in refining graft designs to achieve optimal false lumen exclusion while maintaining vital organ perfusion.
Durability and Long-term Performance
While immediate deployment and sealing are critical, the long-term performance of stents and grafts is equally important. Aortic dissection models can be adapted to simulate chronic conditions and assess device durability over time.
Aspects of long-term performance that can be evaluated include:
- Material fatigue and wear
- Resistance to migration or displacement
- Maintenance of patency and flow dynamics
By subjecting devices to simulated pulsatile flow and mechanical stress, researchers can predict how stents and grafts will perform in the dynamic environment of the aorta. This information is crucial for developing devices that not only provide immediate therapeutic benefits but also offer long-lasting solutions for patients with aortic dissections.
Accelerating Innovation Through Realistic Procedural Feedback
Aortic dissection models serve as powerful tools for accelerating innovation in medical device development by providing realistic procedural feedback. This invaluable insight allows researchers and engineers to refine their designs and techniques, ultimately leading to more effective and safer interventional solutions.
Enhancing Delivery System Design
One of the key areas where realistic procedural feedback proves invaluable is in the design of delivery systems for aortic dissection devices. These models allow developers to simulate the entire deployment process, from initial insertion to final positioning.
Aspects of delivery system design that can be optimized include:
- Catheter flexibility and trackability
- Precise control during deployment
- Ease of device retrieval or repositioning
By using models that accurately replicate the tortuosity of the aortic arch and the challenging anatomy of dissected segments, engineers can identify potential issues with delivery systems early in the development process. This feedback enables iterative improvements, resulting in more user-friendly and reliable deployment mechanisms.
Refining Procedural Techniques
Aortic dissection models provide a platform for refining and developing new procedural techniques. These simulations allow interventionalists to practice and perfect their approaches in a risk-free environment.
Areas where procedural techniques can be refined include:
- Guidewire navigation through complex dissection flaps
- Optimal positioning of fenestrated or branched grafts
- Management of challenging anatomical variations
By offering a realistic representation of various aortic dissection scenarios, these models enable the development of standardized procedural protocols. This not only enhances the skills of individual practitioners but also contributes to the overall advancement of endovascular techniques for treating aortic dissections.
Facilitating Collaborative Innovation
The use of aortic dissection models in device development fosters collaborative innovation among various stakeholders in the medical field. These models serve as a common platform for discussion and idea exchange between device engineers, interventional radiologists, vascular surgeons, and other specialists.
Benefits of this collaborative approach include:
- Integration of clinical insights into device design
- Identification of unmet needs in current treatment options
- Cross-disciplinary problem-solving for complex cases
By bringing together diverse expertise around a tangible, realistic model, innovative solutions can emerge more rapidly. This collaborative environment accelerates the development of novel approaches to managing aortic dissections, potentially leading to breakthroughs in treatment strategies and device technologies.
Conclusion
Aortic dissection models play a pivotal role in advancing medical device development, offering a realistic and versatile platform for innovation. These models facilitate comprehensive preclinical testing, enable detailed evaluation of stents and grafts, and provide invaluable procedural feedback. By bridging the gap between conceptual design and clinical application, they significantly accelerate the development of safer, more effective interventional technologies. As the field of endovascular treatment for aortic dissections continues to evolve, these sophisticated simulations will remain essential tools in driving progress and improving patient outcomes.
Contact Us
For more information on our advanced aortic dissection models and how they can benefit your research or device development projects, please contact Trandomed. Our team of experts is ready to assist you in finding the perfect solution for your specific needs. Reach out to us at jackson.chen@trandomed.com to explore how our cutting-edge medical simulators can accelerate your innovation process and contribute to the advancement of aortic dissection treatments.
_1736214519364.webp)
_1734504197376.webp)
_1734507815464.webp)
_1732863713705.webp)
_1732843184544.webp)