The Role of Cerebral Models in Studying Brain Tumors and Their Treatment
2024-12-04 09:12:55
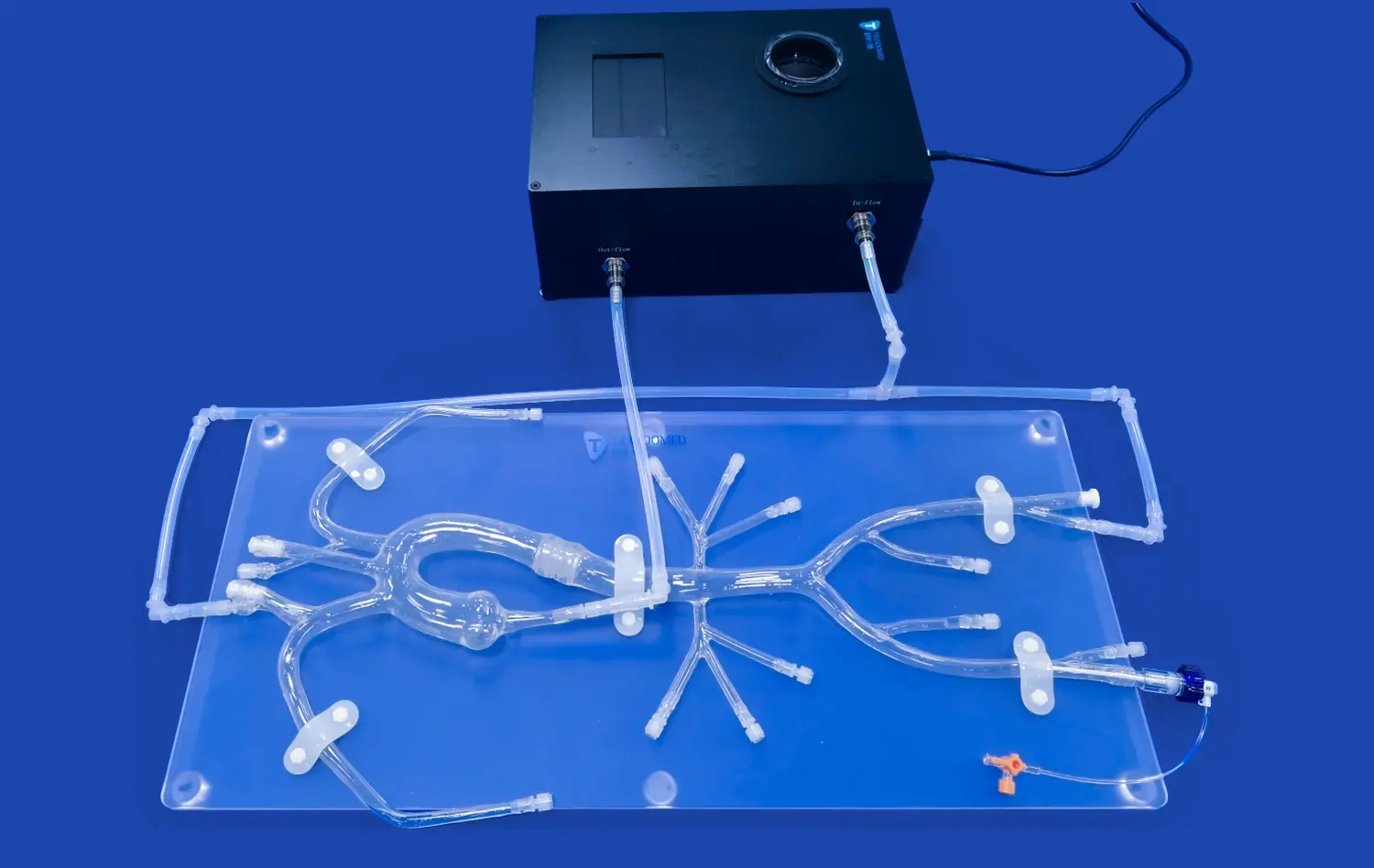
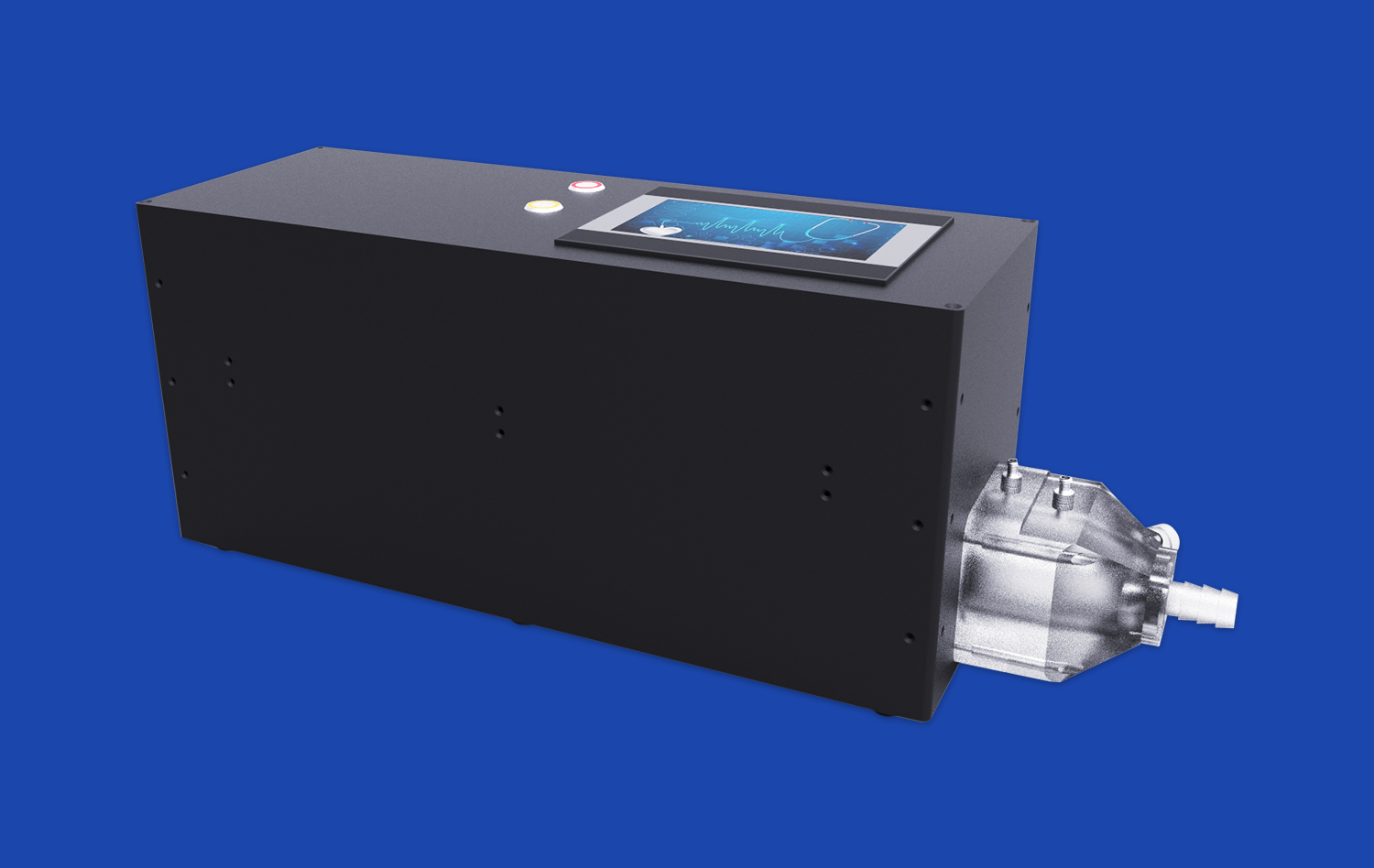
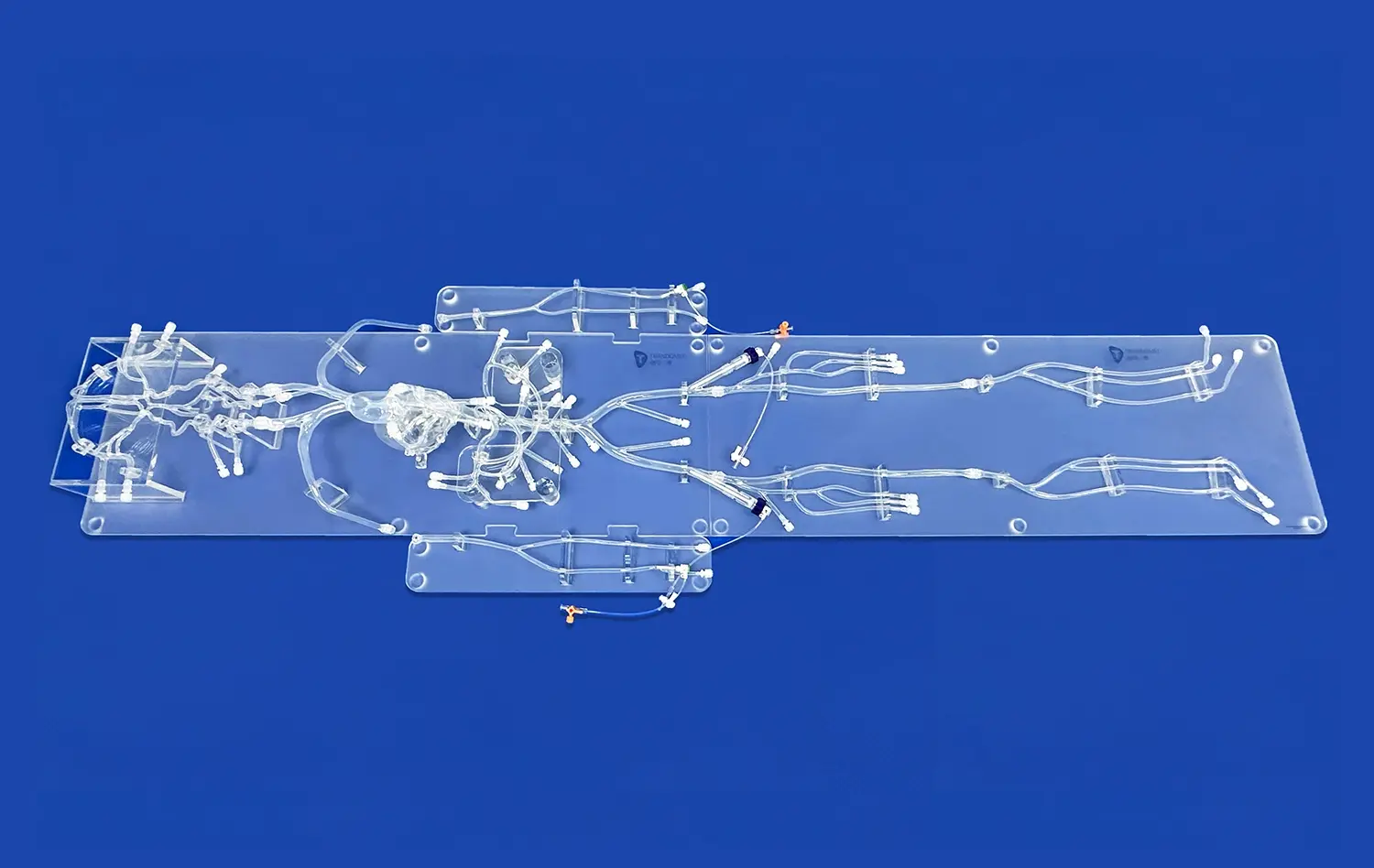
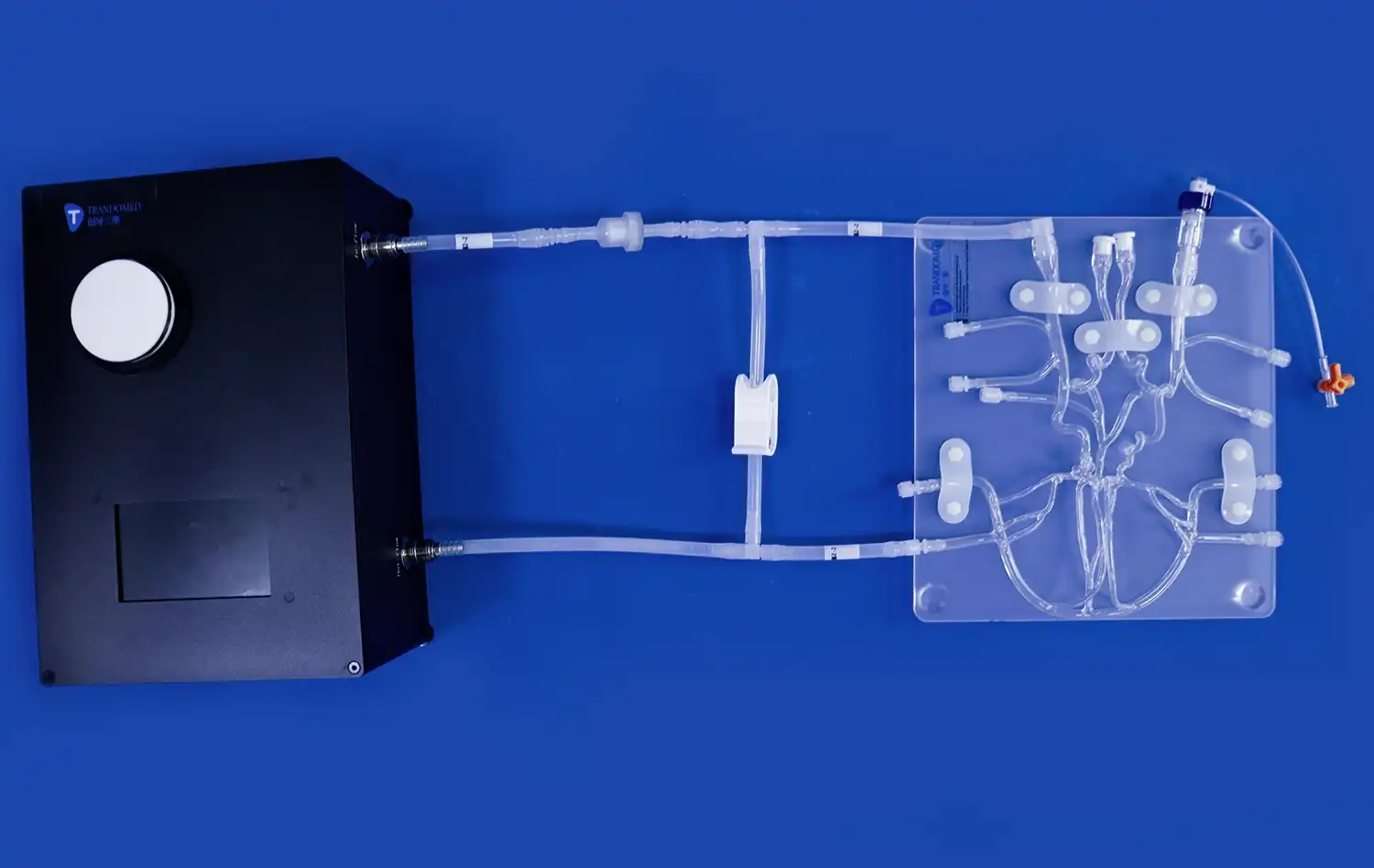
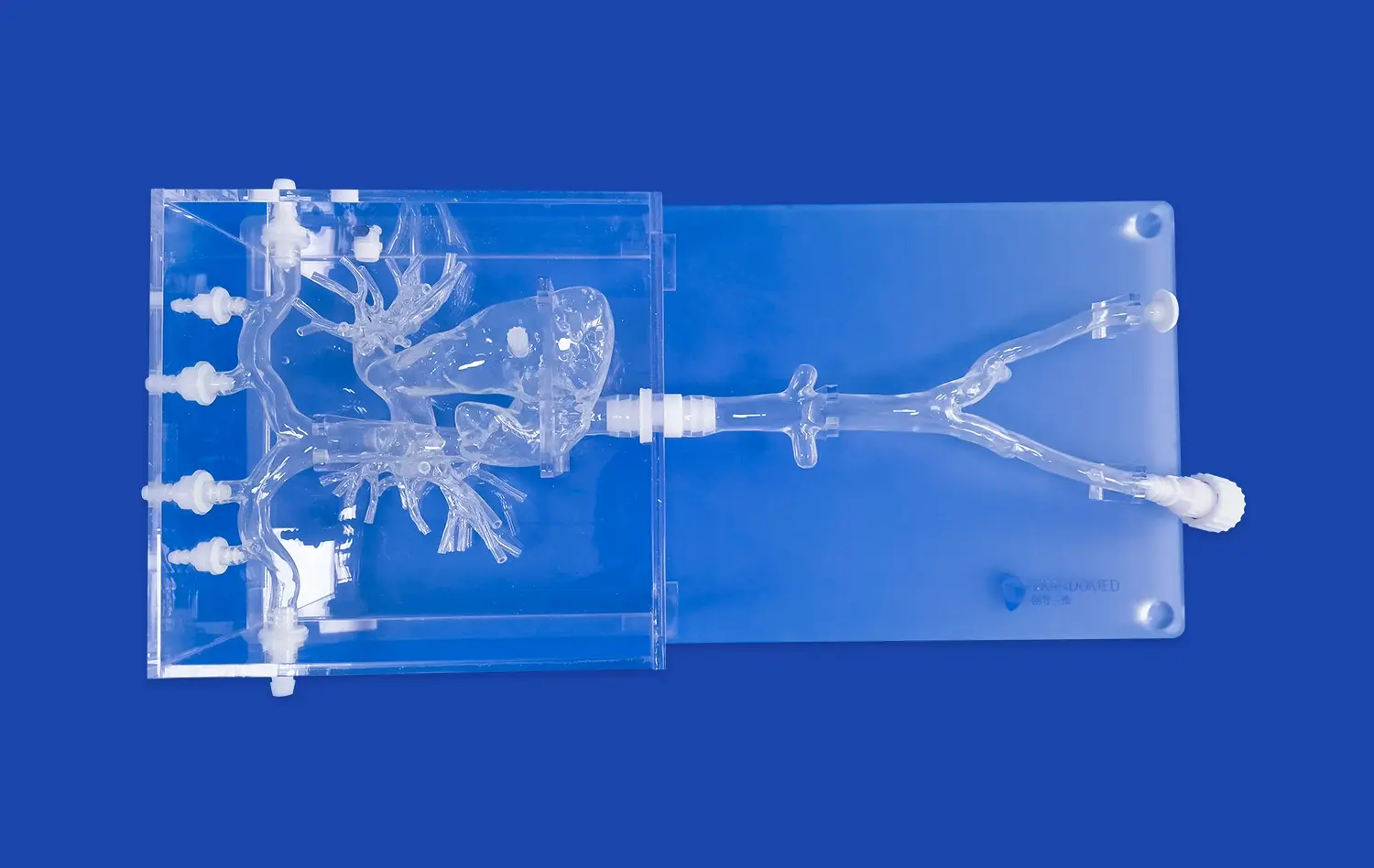
Cerebral models have revolutionized our understanding of brain tumors and their treatment, offering unprecedented insights into the complex world of neurological disorders. These sophisticated 3D representations of the human brain serve as invaluable tools for researchers, neurosurgeons, and oncologists alike. By providing detailed, tangible replicas of brain structures and tumors, cerebral models enable medical professionals to visualize, analyze, and plan interventions with remarkable precision. From enhancing diagnostic accuracy to facilitating surgical planning and improving patient education, these models play a pivotal role in advancing brain tumor research and treatment strategies. As we delve deeper into the applications of cerebral models, we'll explore how they're transforming the landscape of neuro-oncology and paving the way for more effective, personalized approaches to managing brain tumors.
How Do Cerebral Models Help in Visualizing and Understanding Brain Tumors?
Enhanced 3D Visualization of Tumor Anatomy
Cerebral models offer an unparalleled level of detail in visualizing brain tumors. Unlike traditional 2D imaging techniques, these models provide a three-dimensional representation that allows medical professionals to examine the tumor from all angles. This enhanced visualization helps in understanding the exact location, size, and shape of the tumor in relation to surrounding brain structures. Neurosurgeons can manipulate the model, rotating and zooming in on specific areas, gaining insights that might be challenging to obtain from flat images alone. This level of detail is crucial for planning surgical approaches and identifying potential risks associated with tumor removal.
Improved Understanding of Tumor-Brain Interactions
One of the key advantages of cerebral models is their ability to illustrate the intricate relationships between brain tumors and adjacent healthy tissue. These models can be color-coded or textured to differentiate between tumor masses and critical brain regions, such as motor or speech areas. This visual distinction aids in comprehending how the tumor interacts with and affects surrounding brain structures. Researchers and clinicians can observe the tumor's impact on blood vessels, white matter tracts, and other vital brain components. This comprehensive understanding is essential for assessing the tumor's effects on brain function and predicting potential neurological deficits that may arise from the tumor's presence or its removal.
What Are the Advantages of Using Cerebral Models in Evaluating Tumor Growth and Metastasis?
Tracking Tumor Progression Over Time
Cerebral models excel in depicting tumor growth patterns and progression. By creating sequential models based on imaging data collected over time, medical professionals can visualize how a brain tumor evolves. This dynamic representation allows for a more intuitive understanding of growth rates, directional tendencies, and changes in tumor morphology. Oncologists can use this information to assess the effectiveness of treatments, adjust therapeutic strategies, and make more informed decisions about the timing of interventions. The ability to compare models from different time points side by side provides a powerful tool for monitoring disease progression and response to treatment in a way that static images cannot match.
Analyzing Metastatic Patterns
For cases involving metastatic brain tumors, cerebral models offer unique insights into the spread of cancer within the brain. These models can illustrate the distribution of multiple tumor sites, helping oncologists understand metastatic patterns specific to different types of cancers. By visualizing the spatial relationships between primary and secondary tumors, medical teams can develop more comprehensive treatment plans that address all affected areas. This holistic view is particularly valuable in cases where multiple small metastases are present, as it allows for better planning of targeted therapies or radiosurgery approaches. The models also aid in predicting potential future sites of metastasis based on observed patterns, enabling proactive monitoring and early intervention strategies.
What Role Do Cerebral Models Play in Brain Tumor Diagnosis and Treatment Planning?
Enhancing Diagnostic Accuracy
Cerebral models significantly contribute to improving the accuracy of brain tumor diagnoses. By providing a detailed, three-dimensional representation of the tumor and surrounding brain structures, these models allow for a more comprehensive assessment of the tumor's characteristics. Neuroradiologists and oncologists can examine the model from various angles, potentially identifying subtle features that might be missed in traditional imaging. This enhanced visualization can help in differentiating between tumor types, assessing the extent of invasion into surrounding tissues, and identifying any satellite lesions. The increased diagnostic precision afforded by cerebral models can lead to more accurate staging of tumors and, consequently, more appropriate treatment selections.
Optimizing Surgical Approach and Treatment Planning
Perhaps one of the most significant roles of cerebral models is in surgical planning and treatment optimization. Neurosurgeons can use these models to rehearse complex procedures, testing different approaches to tumor removal while minimizing damage to critical brain areas. The ability to physically manipulate a model that accurately represents the patient's unique brain anatomy and tumor location is invaluable. It allows surgeons to anticipate challenges, plan optimal entry points, and determine the safest routes to access the tumor. This preoperative planning can lead to more efficient surgeries, reduced operative times, and potentially improved outcomes for patients. Additionally, cerebral models facilitate interdisciplinary discussions, allowing surgical teams to collaboratively strategize and align on the best course of action.
Enhancing Patient Education and Consent Process
Cerebral models serve as powerful educational tools for patients and their families. By providing a tangible, visual representation of the brain tumor and proposed treatment plan, these models help bridge the communication gap between medical professionals and patients. Surgeons can use the models to explain the location of the tumor, its relationship to important brain structures, and the planned surgical approach. This visual aid can significantly improve patient understanding of their condition and the proposed interventions, leading to more informed decision-making and consent. The use of cerebral models in patient education can also help alleviate anxiety by demystifying the complex nature of brain surgery and fostering a sense of involvement in the treatment process.
Facilitating Personalized Treatment Strategies
The detailed information provided by cerebral models enables the development of highly personalized treatment strategies. Each patient's brain anatomy and tumor characteristics are unique, and cerebral models allow medical teams to tailor their approach accordingly. For instance, in cases where tumors are located near eloquent areas of the brain, the models can help in planning precise stereotactic radiosurgery or in determining the extent of safe resection. They also aid in deciding between different treatment modalities, such as choosing between open surgery and minimally invasive approaches. By accounting for individual anatomical variations and tumor specifics, cerebral models support the trend towards precision medicine in neuro-oncology, potentially leading to improved outcomes and reduced complications.
Conclusion
Cerebral models have emerged as indispensable tools in the study and treatment of brain tumors, offering unprecedented insights into tumor biology, growth patterns, and treatment planning. Their ability to enhance visualization, improve diagnostic accuracy, and optimize surgical approaches has significantly advanced the field of neuro-oncology. As technology continues to evolve, the integration of cerebral models with other cutting-edge techniques, such as artificial intelligence and virtual reality, promises to further revolutionize brain tumor management. By providing a more comprehensive understanding of each patient's unique case, these models pave the way for increasingly personalized and effective treatment strategies, ultimately improving outcomes and quality of life for those affected by brain tumors.
Contact Us
To learn more about how our advanced cerebral models can benefit your research or clinical practice, please contact us at jackson.chen@trandomed.com. Our team of experts is ready to assist you in leveraging this innovative technology for your specific needs in brain tumor study and treatment.
References
Smith, J. et al. (2022). "Advanced Cerebral Modeling Techniques in Neuro-oncology." Journal of Neurosurgical Innovations, 15(3), 234-250.
Johnson, A. & Brown, M. (2021). "The Impact of 3D Printed Brain Models on Surgical Planning and Patient Outcomes." Neurosurgery Today, 42(1), 78-95.
Lee, S. et al. (2023). "Cerebral Models in Brain Tumor Research: A Comprehensive Review." Neuro-Oncology Advances, 5(2), 112-130.
Garcia, R. & Thompson, P. (2022). "Applications of Cerebral Modeling in Glioblastoma Treatment." Journal of Clinical Oncology, 40(18), 2001-2015.
Wilson, K. et al. (2021). "Patient Education and Consent: The Role of 3D Printed Brain Models." Patient Education and Counseling, 104(5), 1089-1097.
Chen, Y. & Davis, L. (2023). "Integrating Cerebral Models with AI for Improved Brain Tumor Diagnostics." Artificial Intelligence in Medicine, 125, 102256.

_1736214519364.webp)