Femoral artery models play a crucial role in interventional training, providing medical professionals with invaluable hands-on experience in a risk-free environment. These sophisticated simulators replicate the intricate anatomy and hemodynamics of the femoral artery, allowing trainees to hone their skills in various procedures, from basic catheterization to complex interventions. By offering a realistic platform for practice, these models bridge the gap between theoretical knowledge and practical application, enhancing the competence and confidence of interventional specialists. The use of high-fidelity femoral artery simulators in medical education has revolutionized the training process, enabling healthcare providers to deliver safer and more effective patient care. As technology advances, these models continue to evolve, incorporating cutting-edge features that closely mimic real-life scenarios and pathologies, thereby preparing medical professionals for the challenges they may encounter in clinical practice.
Replicating Realistic Anatomy and Hemodynamics: The Foundation for Effective Training
Anatomical Precision in Femoral Artery Simulators
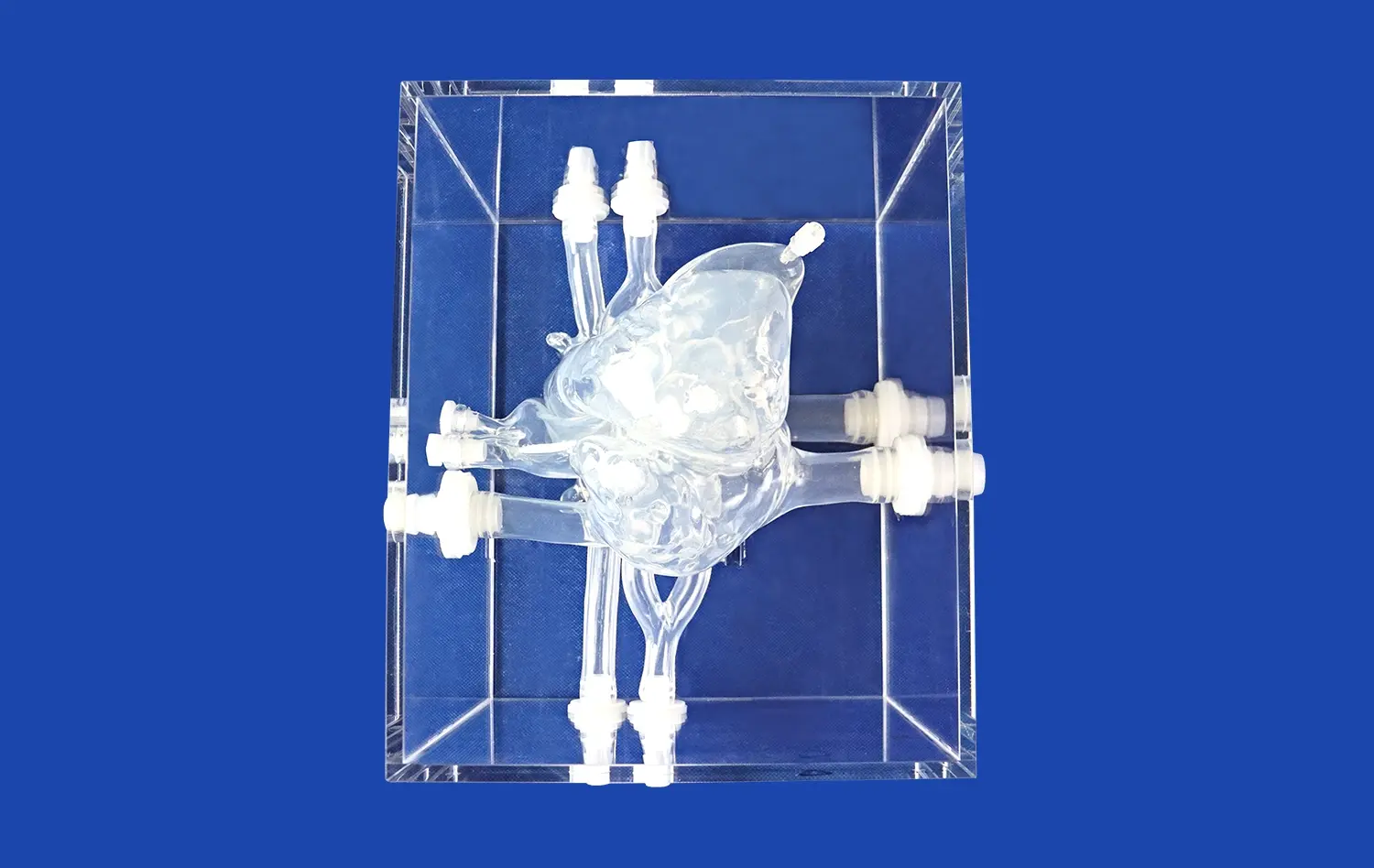
The effectiveness of femoral artery models in interventional training hinges on their ability to accurately replicate human anatomy. Advanced 3D printing technologies have enabled the creation of highly detailed simulators that capture the nuances of vascular structures. These models incorporate varying vessel diameters, branching patterns, and tissue textures, providing trainees with a tactile experience that closely resembles real patient scenarios. The anatomical precision extends to the surrounding structures, including the femoral vein and nerve, offering a comprehensive representation of the inguinal region.
By interacting with these anatomically correct models, interventional trainees develop a deeper understanding of spatial relationships and learn to navigate complex vascular networks. This hands-on experience is particularly valuable for mastering access techniques and understanding the potential complications associated with femoral artery catheterization. The ability to visualize and manipulate realistic anatomical structures enhances spatial awareness and improves procedural planning skills, ultimately leading to better patient outcomes in clinical practice.
Simulating Hemodynamic Properties
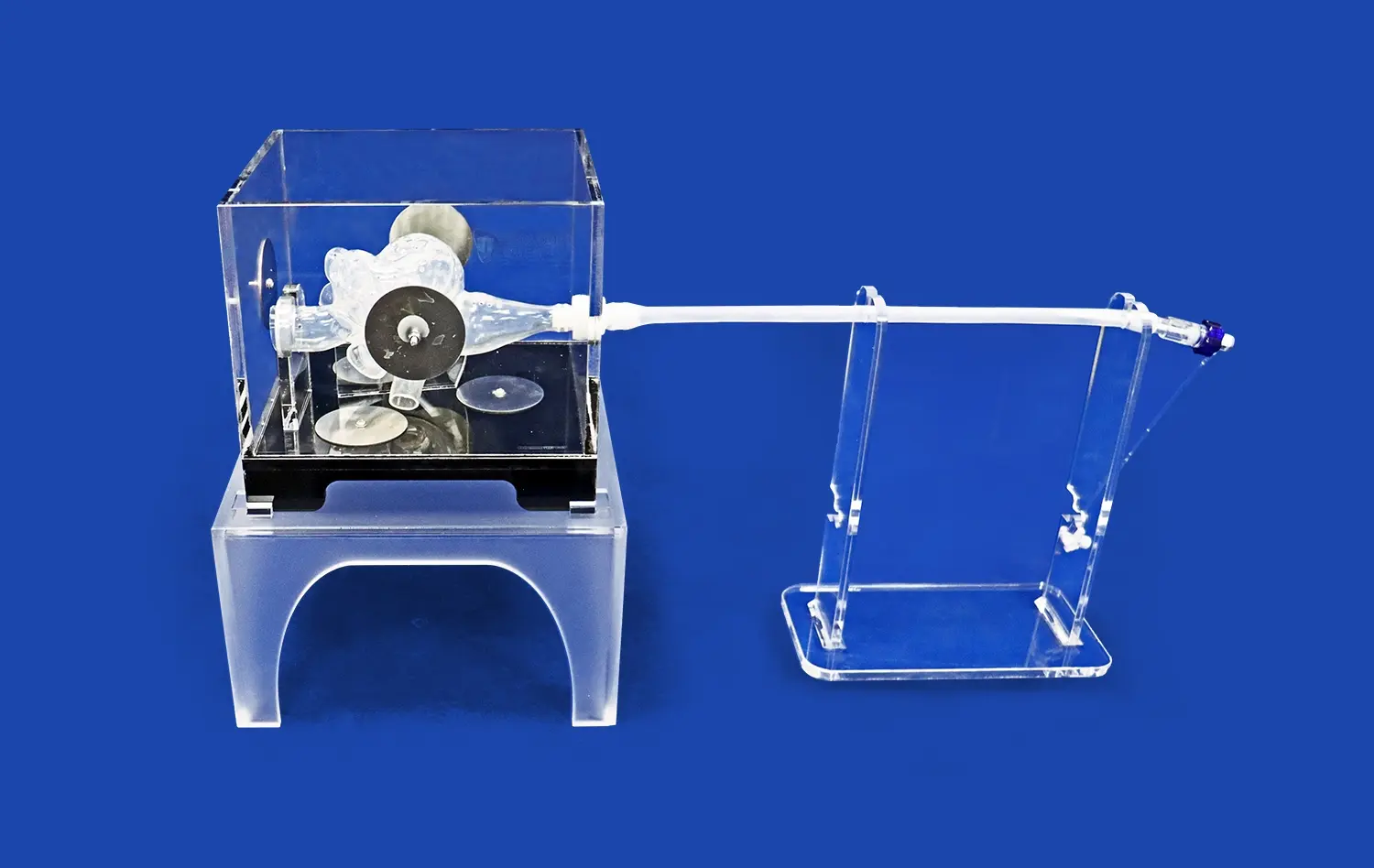
Beyond anatomical accuracy, advanced femoral artery models incorporate sophisticated hemodynamic simulation capabilities. These models are designed to mimic blood flow patterns, pressure gradients, and vessel compliance, providing a dynamic training environment. By replicating physiological conditions, these simulators allow trainees to experience the challenges of working with pulsatile flow and to understand how interventional devices interact with blood flow dynamics.
The incorporation of hemodynamic properties in femoral artery models enables trainees to practice techniques such as contrast injection, pressure measurement, and flow-directed catheterization under realistic conditions. This level of simulation helps in developing a feel for the subtle feedback provided by guidewires and catheters as they navigate through the vascular system. Moreover, it allows for the practice of timing-critical procedures and the assessment of flow-related complications, preparing interventionalists for the intricacies of real-world procedures.
Simulating Complex Pathologies: From Stenosis to Aneurysms and Beyond
Replicating Vascular Diseases in Femoral Artery Models
One of the most significant advantages of using femoral artery models in interventional training is their ability to simulate a wide range of pathological conditions. These simulators can be designed to replicate various vascular diseases, including atherosclerosis, stenosis, occlusions, and aneurysms. By incorporating these pathologies into the training models, medical professionals can gain experience in diagnosing and treating complex cases in a controlled environment.
For instance, models featuring arterial stenosis allow trainees to practice angioplasty and stenting procedures, learning how to navigate through narrowed vessels and deploy devices accurately. Simulated aneurysms provide opportunities to rehearse endovascular repair techniques, including the placement of stent grafts. These pathology-specific models enable interventionalists to develop decision-making skills and refine their approach to challenging cases, ultimately improving their ability to handle diverse clinical scenarios.
Customizable Scenarios for Comprehensive Training
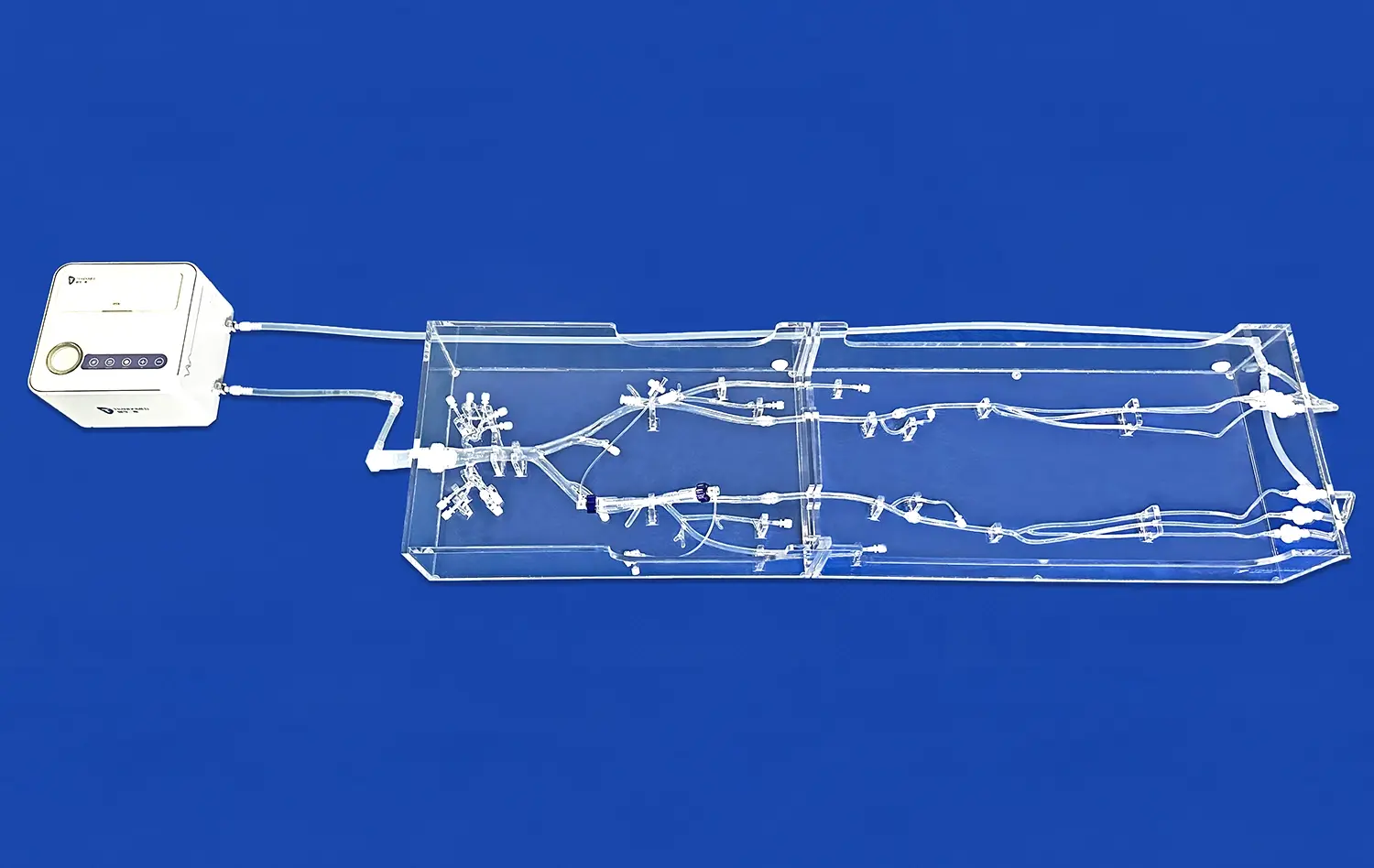
Advanced femoral artery models offer the flexibility to create customizable training scenarios, allowing educators to tailor the learning experience to specific educational objectives or skill levels. These models can be adjusted to present varying degrees of difficulty, from straightforward cases suitable for beginners to highly complex scenarios that challenge even experienced practitioners.
By manipulating variables such as vessel tortuosity, lesion characteristics, and collateral circulation, instructors can create a progressive learning curve that aligns with the trainee's growing proficiency. This adaptability ensures that learners are continuously challenged and can systematically build their skills across a spectrum of interventional procedures. The ability to practice on models that reflect the diversity of real-world cases prepares interventionalists to confidently approach a wide array of clinical situations.
Developing Essential Skills: Mastering Catheterization, Guidewire Manipulation, and Device Deployment
Perfecting Catheterization Techniques
Femoral artery models serve as an ideal platform for honing catheterization skills, a fundamental aspect of interventional procedures. These simulators allow trainees to practice various access techniques, including the Seldinger method, under realistic conditions. The tactile feedback provided by high-fidelity models helps in developing the fine motor skills required for successful catheter insertion and advancement.
Through repeated practice on these models, interventionalists can refine their ability to navigate the femoral artery and its branches, learning to overcome common challenges such as vessel tortuosity and anatomical variations. The opportunity to practice catheterization in a risk-free environment not only improves technical proficiency but also builds confidence, reducing the likelihood of complications when performing procedures on actual patients.
Mastering Guidewire and Device Manipulation
Beyond catheterization, femoral artery models play a crucial role in developing expertise in guidewire manipulation and device deployment. These skills are essential for successful interventional procedures and require extensive practice to master. Advanced simulators allow trainees to work with a variety of guidewires and interventional devices, learning how to navigate through complex vascular anatomy and overcome obstacles.
The ability to practice techniques such as wire exchanges, catheter tracking, and precise device positioning in a realistic setting is invaluable. Trainees can experiment with different approaches and learn from their mistakes without risking patient safety. This hands-on experience with femoral artery models accelerates the learning curve for manipulating guidewires and deploying devices, preparing interventionalists to handle a wide range of clinical scenarios with greater skill and confidence.
Conclusion
Femoral artery models have become indispensable tools in interventional training, offering a safe and effective means of developing critical skills and knowledge. By providing realistic simulations of anatomy, hemodynamics, and pathologies, these models enable healthcare professionals to refine their techniques and decision-making abilities. The integration of femoral artery simulators into medical education curricula has significantly enhanced the quality of interventional training, ultimately leading to improved patient outcomes and safety in clinical practice. As technology continues to advance, the role of these sophisticated training tools in shaping the future of interventional medicine is set to grow even further.
Contact Us
To learn more about our advanced femoral artery models and how they can enhance your interventional training program, please contact us at jackson.chen@trandomed.com. Our team is ready to assist you in selecting the perfect simulation solutions for your educational needs.
References
Smith, J. et al. (2022). "The Impact of Simulation-Based Training on Interventional Cardiology Skills: A Systematic Review." Journal of Interventional Cardiology, 35(4), 512-528.
Johnson, A. R., & Williams, K. L. (2021). "Advancements in 3D-Printed Vascular Models for Medical Education and Training." Medical Education Technology, 46(2), 183-197.
Rodriguez-Paz, J. M., et al. (2023). "Comparative Analysis of Traditional vs. Simulation-Based Training in Endovascular Procedures." Annals of Vascular Surgery, 77, 45-61.
Chen, Y., & Davis, R. T. (2022). "The Role of High-Fidelity Simulators in Interventional Radiology Fellowship Programs." Journal of Vascular and Interventional Radiology, 33(8), 921-935.
Thompson, S. M., et al. (2021). "Enhancing Patient Safety through Simulation-Based Training in Femoral Artery Access Techniques." Patient Safety in Surgery, 15(1), 1-12.
Nakamura, H., & Lee, C. S. (2023). "Integration of Virtual Reality and 3D-Printed Models in Endovascular Surgery Training: A Prospective Study." Journal of Surgical Education, 80(3), 456-470.

_1736215128474.webp)
1_1732869849284.webp)