How Do Valve Models Contribute to Safer Surgical Procedures?
Enhanced Surgical Precision through Realistic Simulation
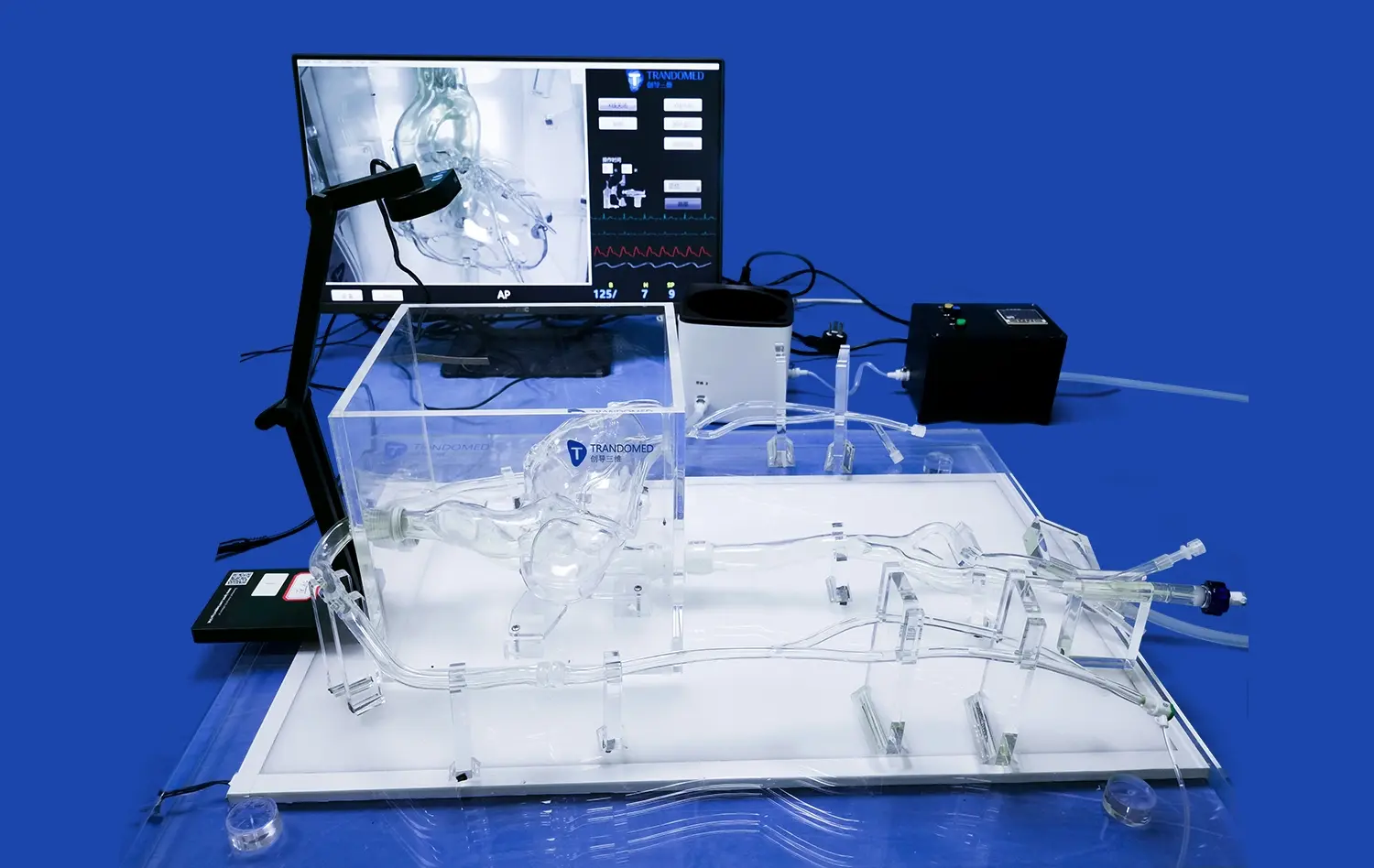
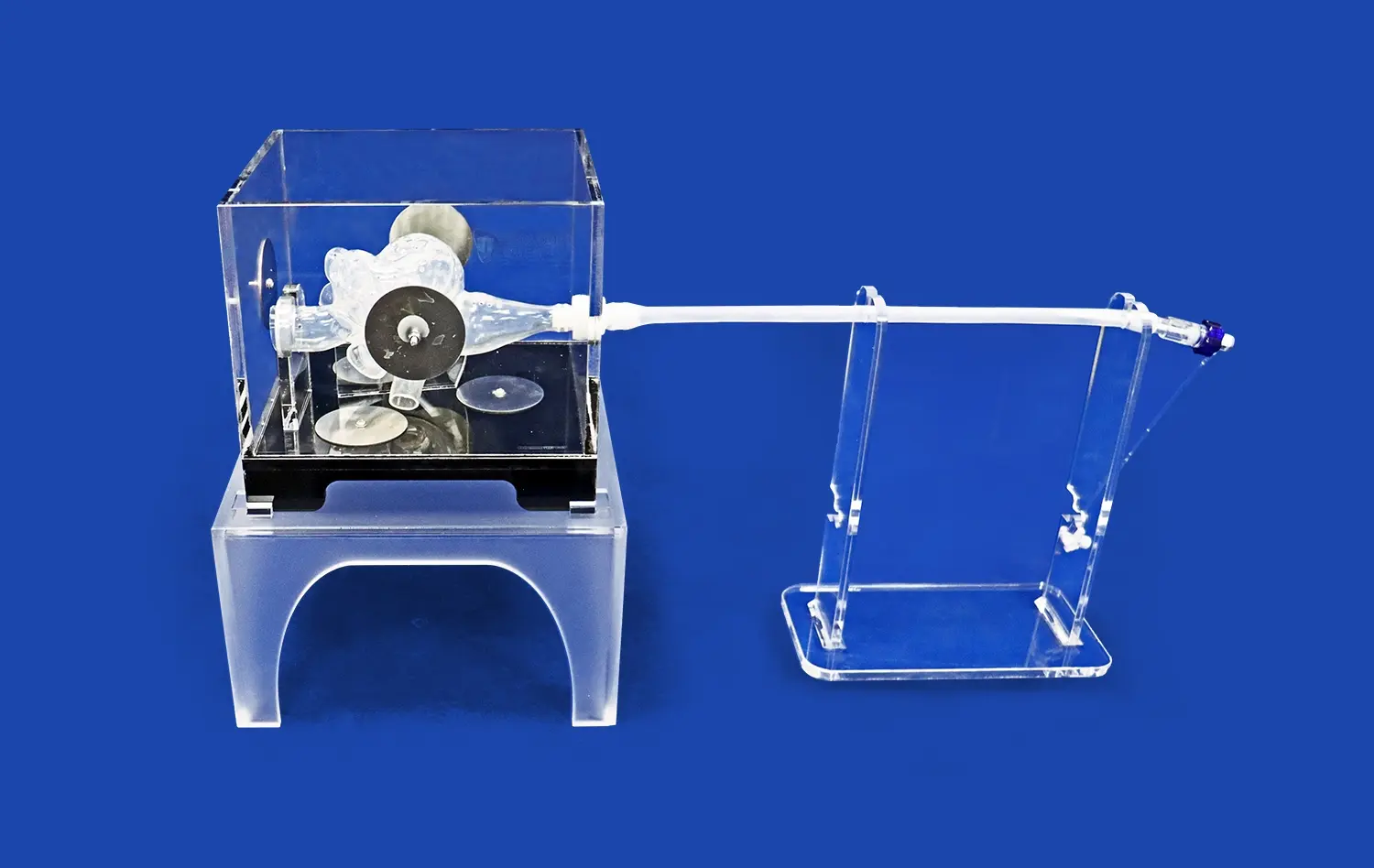
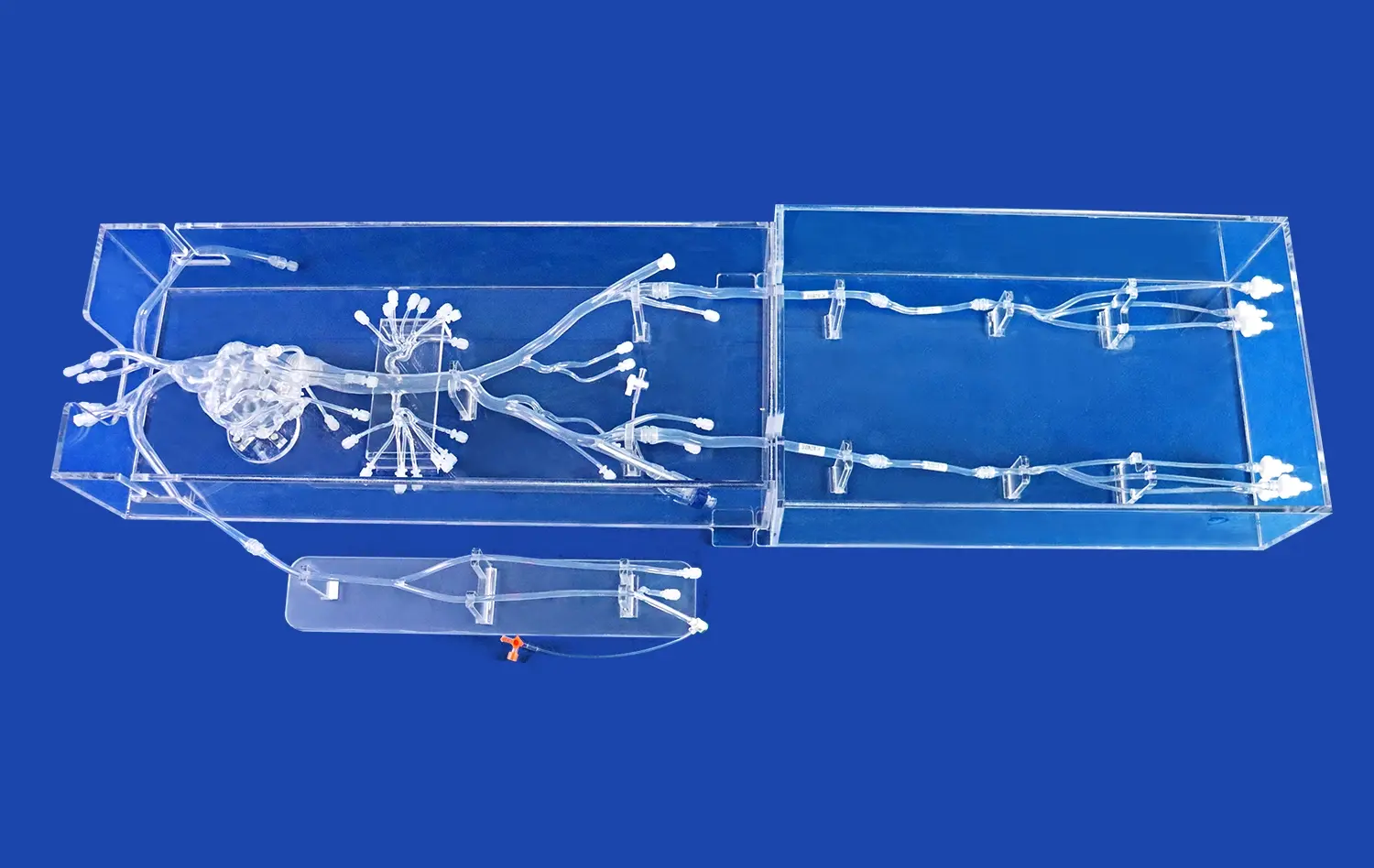
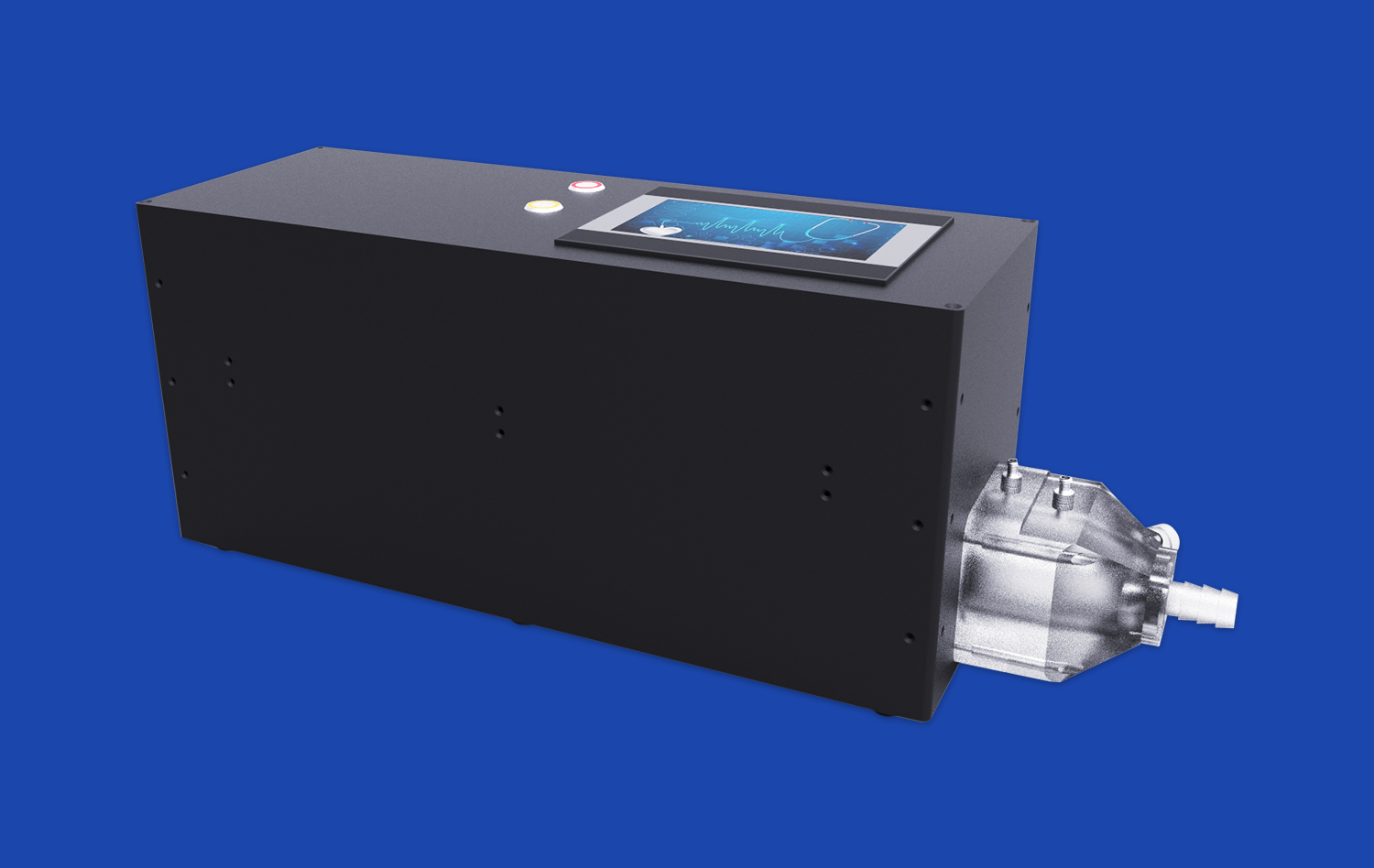
Mitral valve models, such as the advanced Mitral Valve Model (XXD006) offered by Trandomed, provide surgeons with an unparalleled opportunity to hone their skills in a controlled environment. These models, crafted from durable Silicone Shore 40A material, accurately replicate the intricate anatomy of the cardiovascular system, including the mitral valve, left ventricle, and surrounding structures. By practicing on these highly realistic models, surgeons can refine their techniques, improving precision and reducing the risk of complications during actual procedures.
Preoperative Planning and Risk Mitigation
One of the key benefits of utilizing mitral valve models is the ability to conduct thorough preoperative planning. Surgeons can use these models to visualize complex anatomical variations, assess potential challenges, and develop tailored surgical approaches. This level of preparation significantly reduces intraoperative surprises and allows for more efficient and safer procedures. The modular design of advanced models, which allows for detachable and replaceable components, further enhances their utility in simulating various surgical scenarios.
Team Training and Communication
Mitral valve models serve as excellent tools for team-based training and improving communication among surgical staff. By simulating procedures on these models, entire surgical teams can practice coordination, refine their roles, and enhance their collective performance. This collaborative approach to training using valve models contributes to a more cohesive and efficient operating room environment, ultimately leading to safer surgical outcomes for patients.
Practical Applications for Patient-Centered Surgical Planning
Customized Approach to Complex Cases
The ability to customize mitral valve models based on patient-specific data is a game-changer in surgical planning. Companies like Trandomed offer services to tailor the structure of the mitral valve model according to individual patient anatomy, using data from CT scans or other imaging modalities. This personalized approach allows surgeons to develop highly specific strategies for each unique case, particularly beneficial when dealing with complex or rare anatomical variations.
Patient Education and Informed Consent
Mitral valve models serve as powerful educational tools for patients and their families. By using these tangible, three-dimensional representations, healthcare providers can more effectively explain the nature of the patient's condition, the proposed surgical intervention, and potential outcomes. This enhanced understanding facilitates more meaningful discussions about treatment options and risks, leading to a more informed consent process and improved patient engagement in their care journey.
Interdisciplinary Collaboration
The use of mitral valve models fosters collaboration between different medical specialties. Cardiologists, cardiac surgeons, and interventional radiologists can collectively examine these models to develop comprehensive treatment plans. This interdisciplinary approach ensures that patients receive the most appropriate care, taking into account various perspectives and expertise. The clarity and precision of models like the Mitral Valve Model (XXD006) make them invaluable assets for such collaborative efforts.
Optimizing Clinical Outcomes Through Simulation-Based Training
Accelerated Learning Curve for New Techniques
Simulation-based training using mitral valve models significantly accelerates the learning curve for new surgical techniques and technologies. For instance, the Mitral Valve Model (XXD006) can be used to simulate mitral valve replacement (MVR) and regurgitation detection, allowing surgeons to gain proficiency in these procedures without putting patients at risk. This accelerated learning process is particularly crucial in the rapidly evolving field of minimally invasive cardiac surgery, where new approaches and devices are continually being introduced.
Objective Assessment and Skill Validation
Mitral valve models provide an objective platform for assessing and validating surgical skills. Medical institutions can use these models to evaluate the competency of trainees and experienced surgeons alike, ensuring that they meet the required standards of proficiency before performing procedures on patients. This objective assessment contributes to maintaining high standards of care and patient safety across healthcare institutions.
Continuous Professional Development
The availability of high-fidelity mitral valve models supports continuous professional development for cardiac care providers. Experienced surgeons can use these models to refine their skills, explore new techniques, and stay updated with the latest advancements in cardiac surgery. This ongoing practice and learning translate directly into improved clinical outcomes, as healthcare providers maintain and enhance their expertise throughout their careers.
Conclusion
The integration of mitral valve models into medical education, surgical planning, and clinical practice represents a significant advancement in cardiovascular care. These models contribute to safer surgical procedures, enable patient-centered planning, and optimize clinical outcomes through simulation-based training. As technology continues to evolve, the role of these models in improving patient care and safety will undoubtedly expand, ushering in a new era of precision and excellence in cardiac surgery.
Contact Us
For healthcare professionals and institutions seeking to enhance their cardiac care capabilities, Trandomed offers state-of-the-art mitral valve models that combine high precision, durability, and customization options. To learn more about how our models can benefit your practice and improve patient outcomes, please contact us at jackson.chen@trandomed.com. Elevate your cardiac care with Trandomed's innovative simulation solutions.