Top Benefits of Using an Endovascular Intervention Trainer for Neurovascular Simulation
2025-08-07 09:00:01
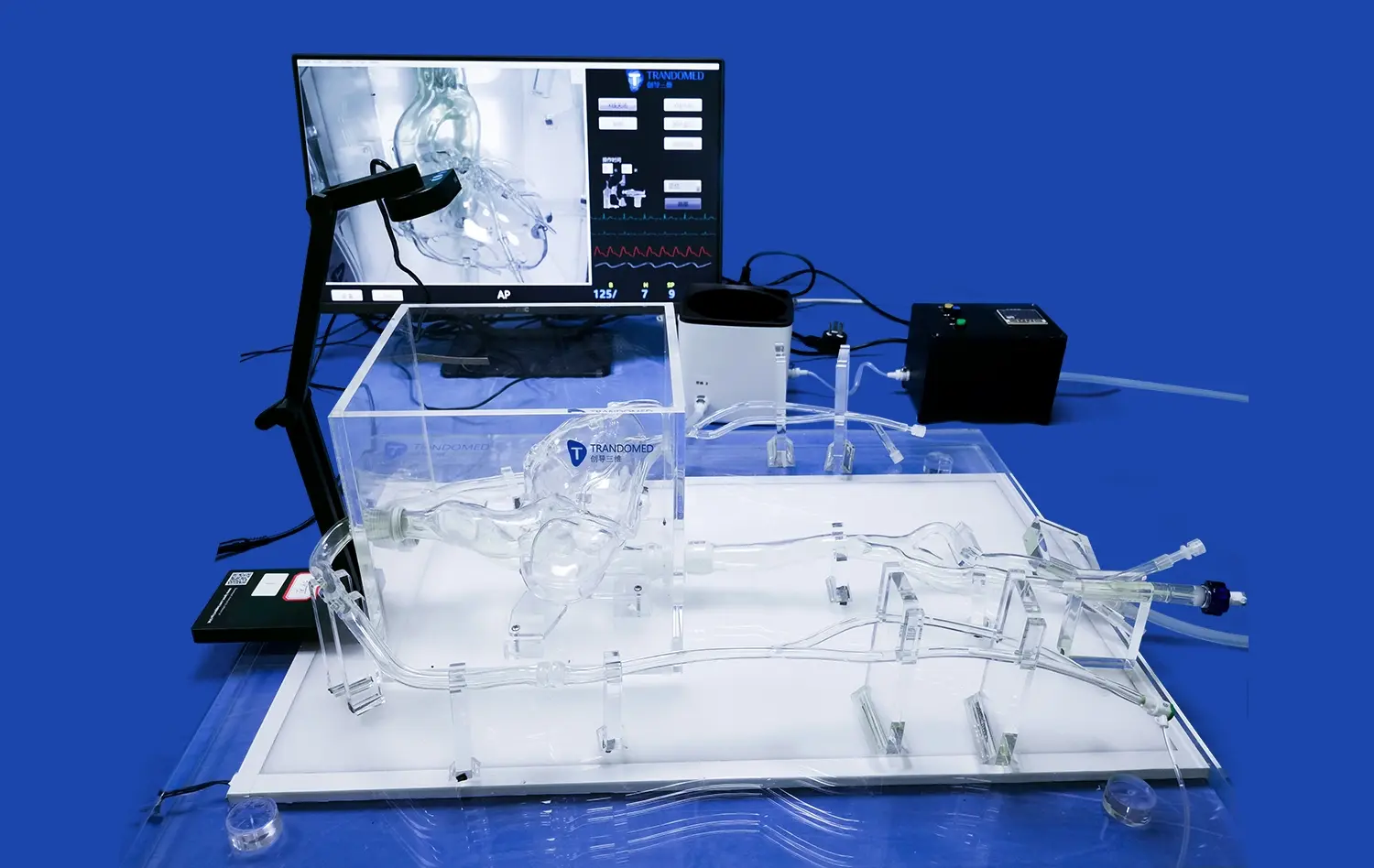
Endovascular intervention trainers have revolutionized medical education and skill development in the field of neurovascular procedures. These advanced simulation systems offer numerous advantages for healthcare professionals, from novice residents to experienced interventionalists. By providing a realistic, risk-free environment for practicing complex neurovascular techniques, endovascular simulators enhance procedural proficiency, improve patient safety, and accelerate the learning curve. Key benefits include hands-on experience with a wide range of clinical scenarios, real-time feedback on performance, and the ability to repeat procedures until mastery is achieved. Additionally, these trainers facilitate team-based training, allowing entire surgical teams to improve their coordination and communication skills. As neurovascular interventions become increasingly sophisticated, the role of high-fidelity simulation in preparing the next generation of specialists has never been more critical.
Why Is Neurovascular Simulation Critical in Medical Training?
Bridging the Gap Between Theory and Practice
Neurovascular simulation provides an indispensable link, effectively translating theoretical concepts learned in lectures and texts into tangible skills within interventional neuroradiology. Conventional educational approaches frequently struggle to offer sufficient, realistic practice for intricate techniques such as aneurysm coiling or mechanical thrombectomy. Endovascular intervention trainers directly address this deficit by enabling trainees to actively utilize their theoretical knowledge within a safe, simulated setting. This experiential learning crucially reinforces cognitive understanding by integrating essential tactile feedback and psychomotor skill development, creating a vital bridge before real-world application on patients.
Enhancing Patient Safety Through Skill Refinement
The paramount importance of patient safety fundamentally underpins all medical training, especially in high-stakes neurovascular interventions where inherent risks exist and even slight procedural errors can lead to devastating outcomes. Simulation-based training offers a critical solution by allowing practitioners to meticulously refine their technical skills and decision-making processes without any risk to actual patients. Through deliberate, repeated practice on sophisticated endovascular simulators and endovascular intervention trainers, interventionalists can master complex maneuvers, optimize device handling, and perfect their techniques. This dedicated rehearsal demonstrably reduces the likelihood of complications and adverse events during subsequent live procedures.
Accelerating the Learning Curve for Complex Procedures
Mastering neurovascular interventions presents a notoriously steep and prolonged learning curve under traditional apprenticeship models. Endovascular trainers significantly expedite this progression by offering unique advantages: immediate, objective feedback on performance, and the ability for rapid, repeated attempts at challenging scenarios. Trainees gain concentrated exposure to a vast spectrum of cases, including uncommon or rare pathologies they might seldom encounter during standard clinical training. This high-density, diverse experience fosters both technical proficiency and clinical confidence far more efficiently than relying solely on observing and gradually assisting in real cases over extended periods.
Realistic Aneurysm and Stroke Scenario Reproduction
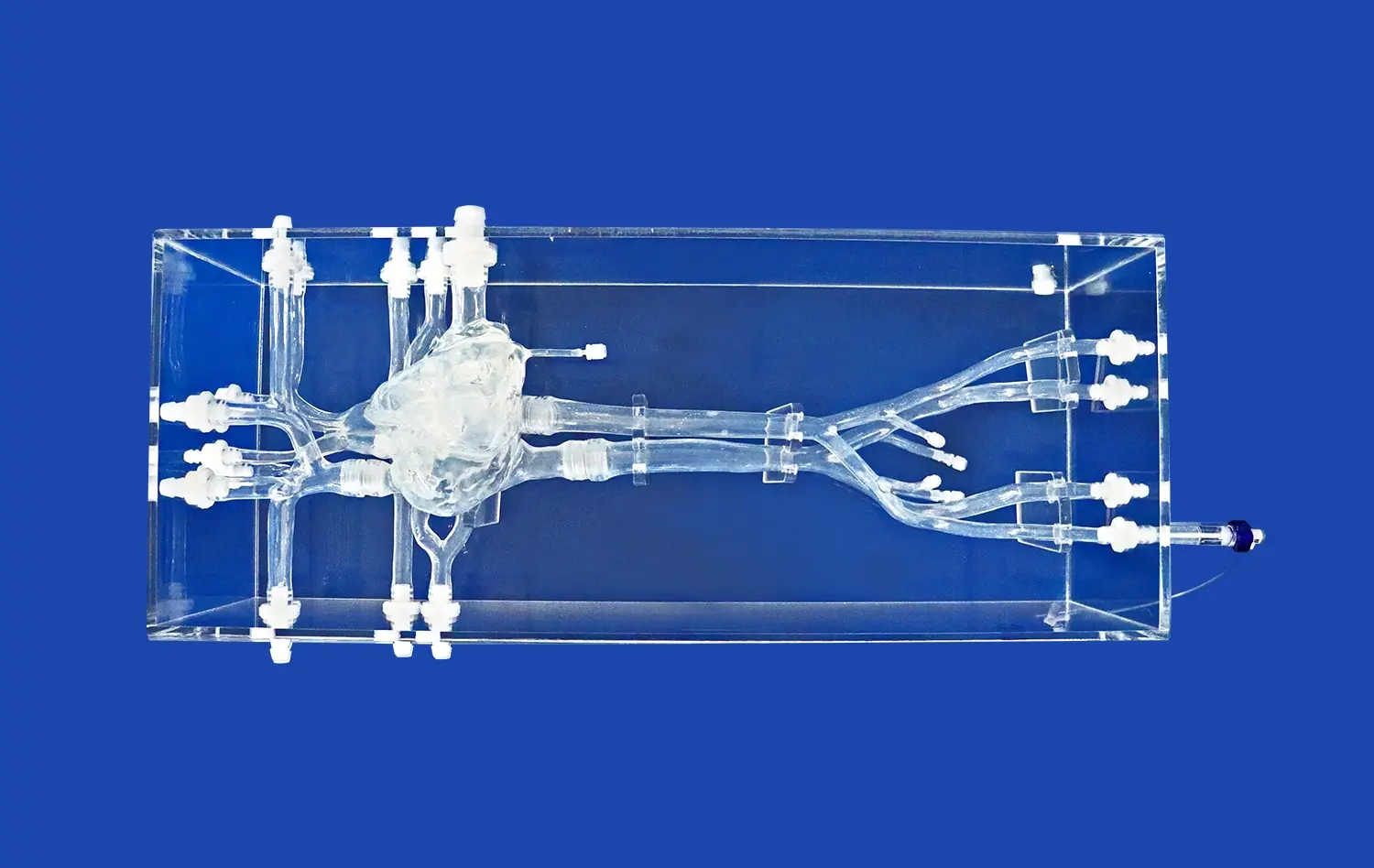
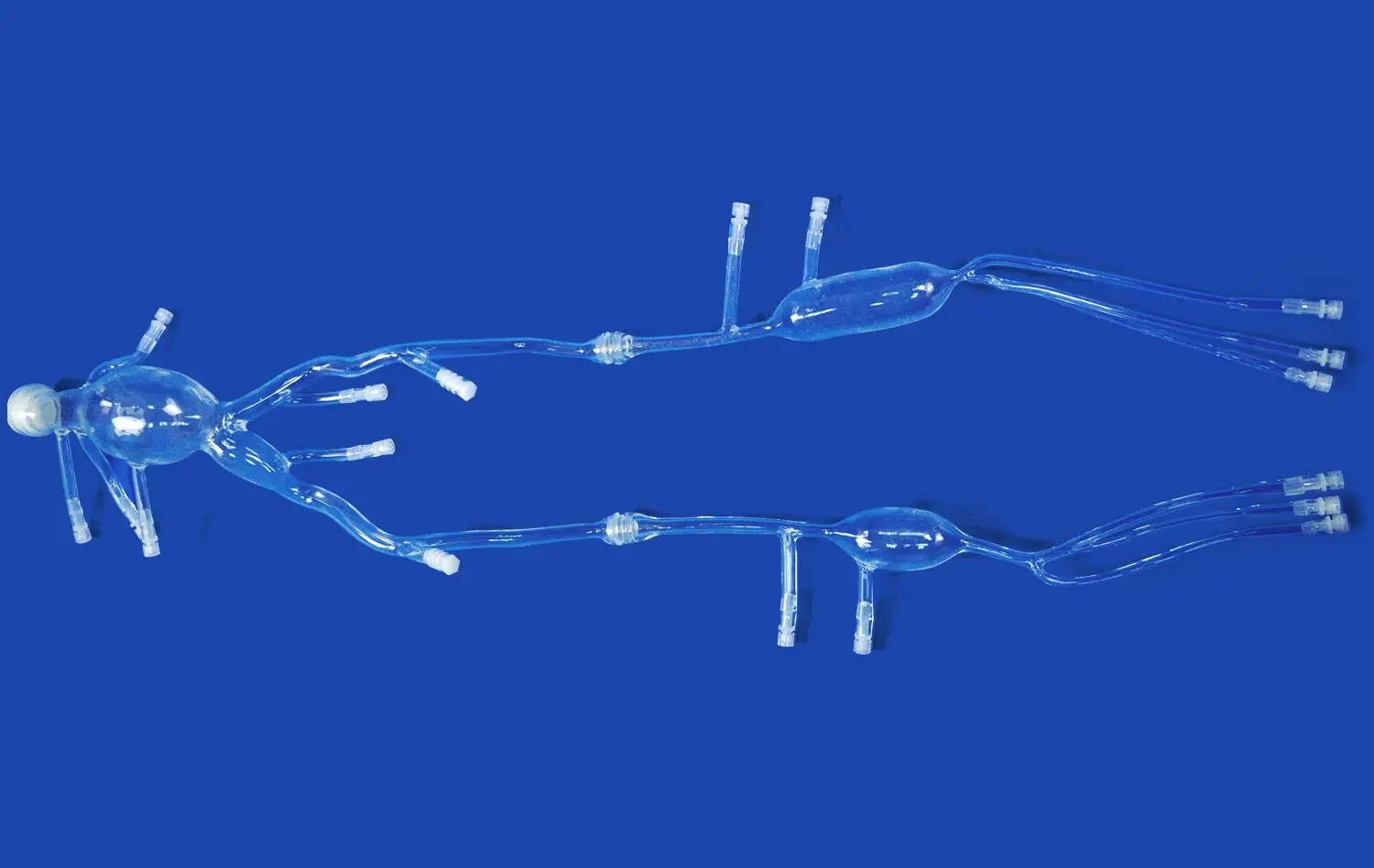
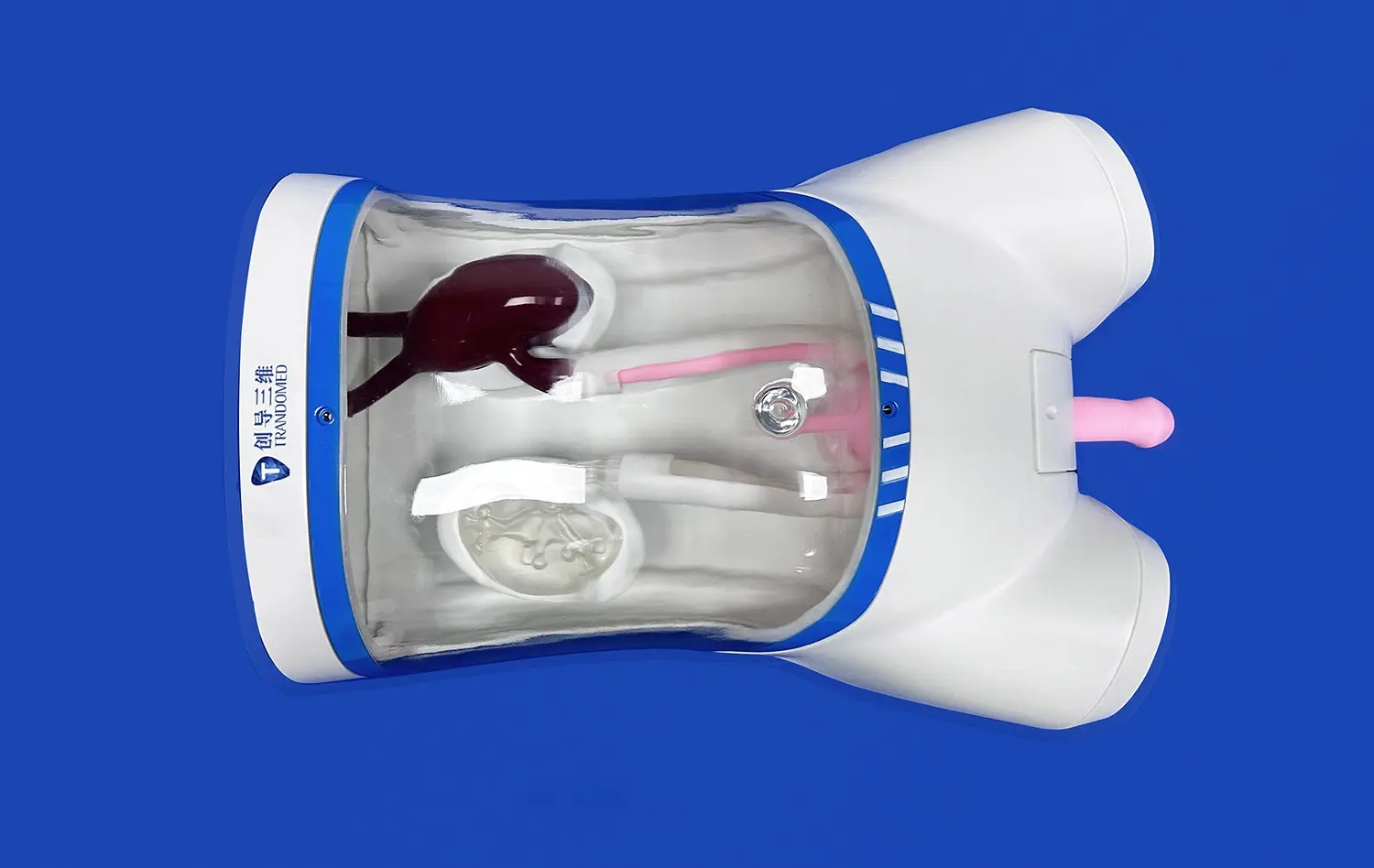
High-Fidelity Anatomical Models
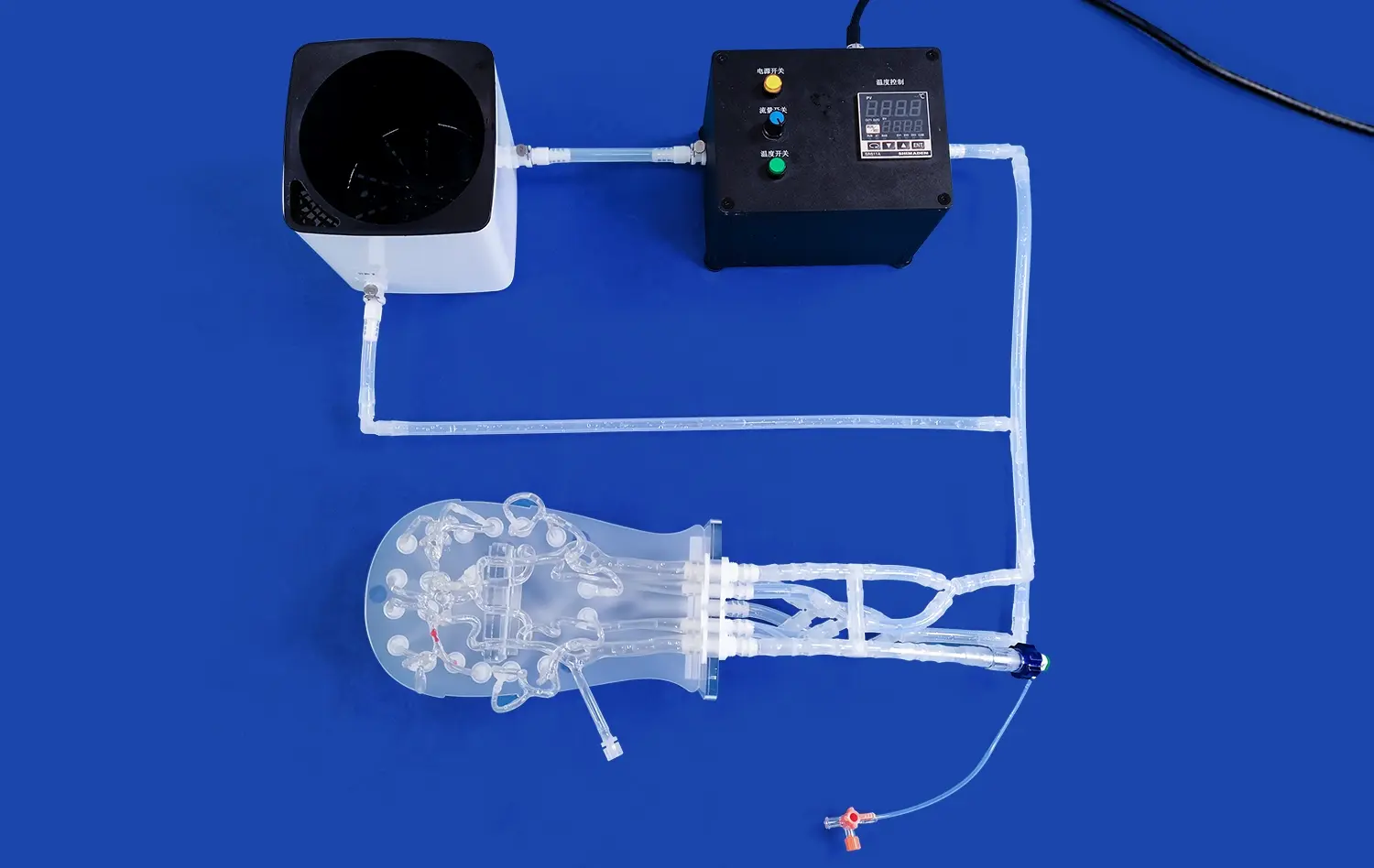
Modern endovascular intervention trainers feature anatomically accurate vascular models based on real patient data. These high-fidelity silicone replicas mimic the elasticity and friction of human blood vessels, providing a tactile experience that closely resembles actual procedures. The ability to work with realistic vessel tortuosity, aneurysm morphologies, and arterial stenoses enhances the transferability of skills from simulation to clinical practice.
Dynamic Flow Simulation
Advanced endovascular intervention trainers incorporate pulsatile flow systems that replicate physiological blood flow patterns. This dynamic environment allows trainees to experience the challenges of catheter navigation and device deployment under realistic hemodynamic conditions. The inclusion of features like variable flow rates and pressure gradients further enhances the fidelity of aneurysm and stroke simulations.
Customizable Pathology Modules
Endovascular trainers often offer modular designs with interchangeable pathology inserts. This flexibility allows educators to create tailored scenarios ranging from simple saccular aneurysms to complex wide-neck bifurcation aneurysms or tandem occlusions in acute ischemic stroke. The ability to customize training modules ensures that learners are exposed to a comprehensive range of clinical challenges.
Improving Device Handling and Team Coordination in Neurointerventions
Mastering Catheter and Wire Techniques
Proficiency in catheter and guidewire manipulation is fundamental to successful neurointerventions. Endovascular simulators provide a safe environment for trainees to develop fine motor skills and tactile sensitivity. Through repeated practice, interventionalists can master techniques such as catheter shaping, wire exchanges, and device deliveries without the pressure of a live clinical setting.
Optimizing Device Selection and Deployment
Neurovascular procedures often require the use of specialized devices such as coils, stents, and flow diverters. Endovascular intervention trainer simulation training allows practitioners to gain familiarity with a wide array of devices and their deployment mechanisms. This experience is invaluable in developing the decision-making skills necessary for optimal device selection and placement in various anatomical and pathological scenarios.
Enhancing Team Communication and Workflow
Effective neurointerventions rely on seamless coordination between multiple team members, including the primary operator, assistant, anesthesiologist, and nursing staff. Endovascular trainers facilitate team-based simulations where entire procedural teams can practice together. This collaborative approach improves communication, refines workflow efficiency, and helps identify and address potential bottlenecks in the interventional process.
Conclusion
The integration of endovascular intervention trainers into neurovascular simulation programs offers substantial benefits for medical education and patient care. These advanced systems provide a realistic, risk-free environment for developing and refining critical skills in neurointerventional procedures. By bridging the gap between theory and practice, enhancing patient safety, and accelerating the learning curve, endovascular simulators play a pivotal role in preparing the next generation of interventionalists. As neurovascular techniques continue to evolve, the importance of high-fidelity simulation in maintaining and advancing practitioner competence cannot be overstated.
Contact Us
Experience the future of neurovascular training with Trandomed's state-of-the-art endovascular intervention trainers. Our customizable simulation systems offer unparalleled realism and versatility, helping healthcare institutions elevate their training programs and improve patient outcomes. To learn more about how Trandomed can revolutionize your neurovascular simulation capabilities, contact us at jackson.chen@trandomed.com.
References
1. Barsuk, J. H., et al. (2019). Simulation-based mastery learning improves patient outcomes in endovascular stroke treatment. Journal of Neurosurgery, 130(4), 1251-1257.
2. Liebig, T., et al. (2018). The impact of virtual reality simulation on the learning curve of aneurysm clipping. World Neurosurgery, 117, e562-e569.
3. Kazemzadeh-Narbat, M., et al. (2020). Engineering approaches to create antibacterial surfaces for biomedical applications. Advanced Materials Interfaces, 7(15), 2000180.
4. Spiotta, A. M., et al. (2017). Impact of a structured neurointerventional fellowship program on patient outcomes: A 10-year analysis. Journal of NeuroInterventional Surgery, 9(1), 30-33.
5. Kreiser, K., et al. (2019). Simulation-based training in endovascular stroke therapy: A systematic review. Clinical Neuroradiology, 29(4), 545-555.
6. Rudarakanchana, N., et al. (2015). Virtual reality simulation for the optimization of endovascular procedures: Current perspectives. Vascular Health and Risk Management, 11, 195-202.