Understanding Coronary Interventions: A Deep Dive into the Cardiovascular Disease Model
2025-06-23 09:00:00
Coronary interventions represent a critical aspect of cardiovascular medicine, offering life-saving treatments for patients with heart disease. The cardiovascular disease model has revolutionized our approach to understanding and treating these complex conditions. This advanced simulation tool provides an unprecedented level of detail, allowing medical professionals to explore intricate arterial structures, practice interventional techniques, and improve patient outcomes. By replicating the nuances of coronary anatomy, including chronic total occlusions (CTOs), stenosis, and calcification, these models serve as invaluable resources for both training and research. As we delve deeper into the world of cardiovascular disease models, we'll uncover how they're transforming the landscape of coronary interventions and enhancing our ability to combat heart disease effectively.
How the Cardiovascular Disease Model Replicates Complex Arterial Structures?
Anatomical Precision in Cardiovascular Simulations
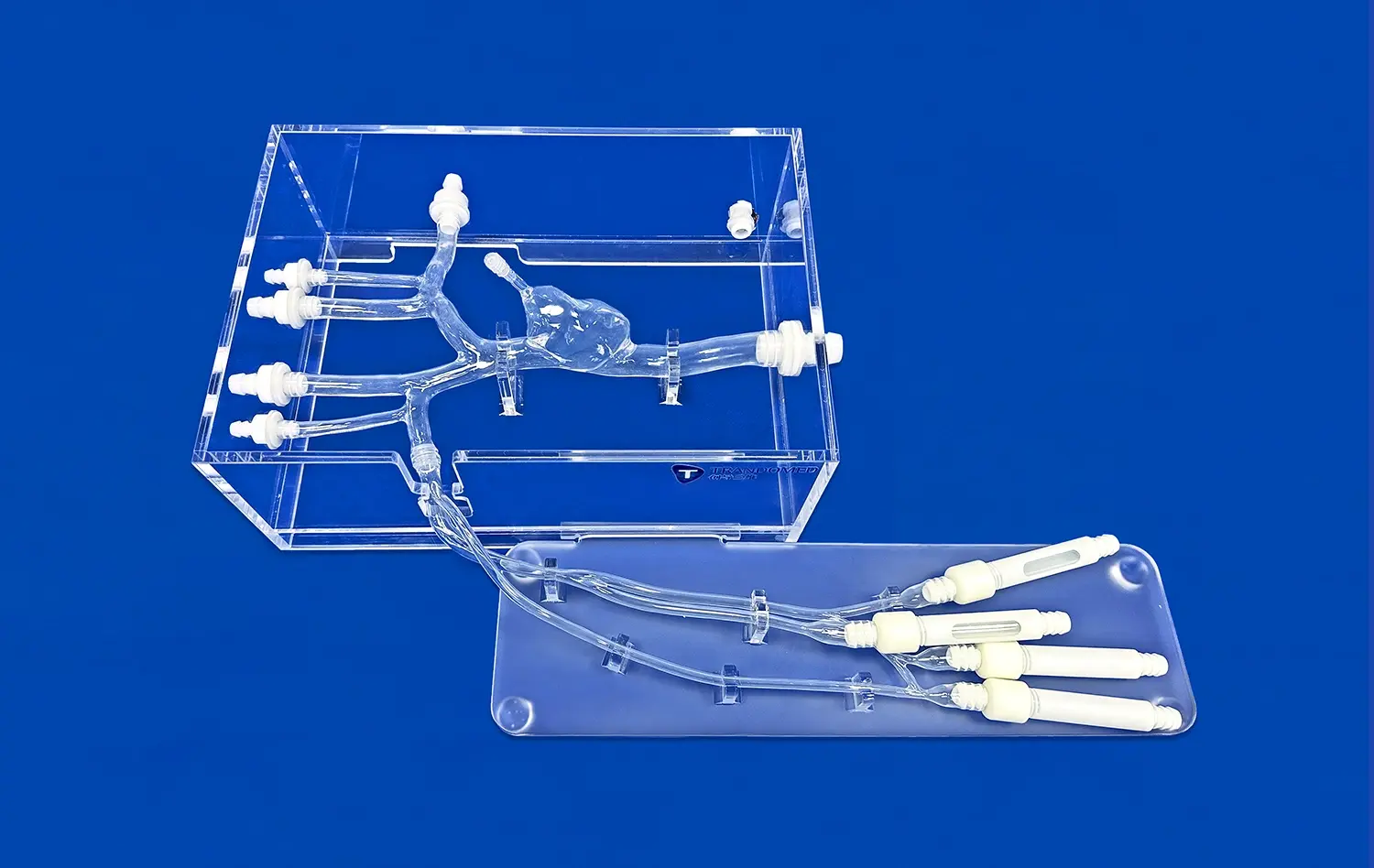
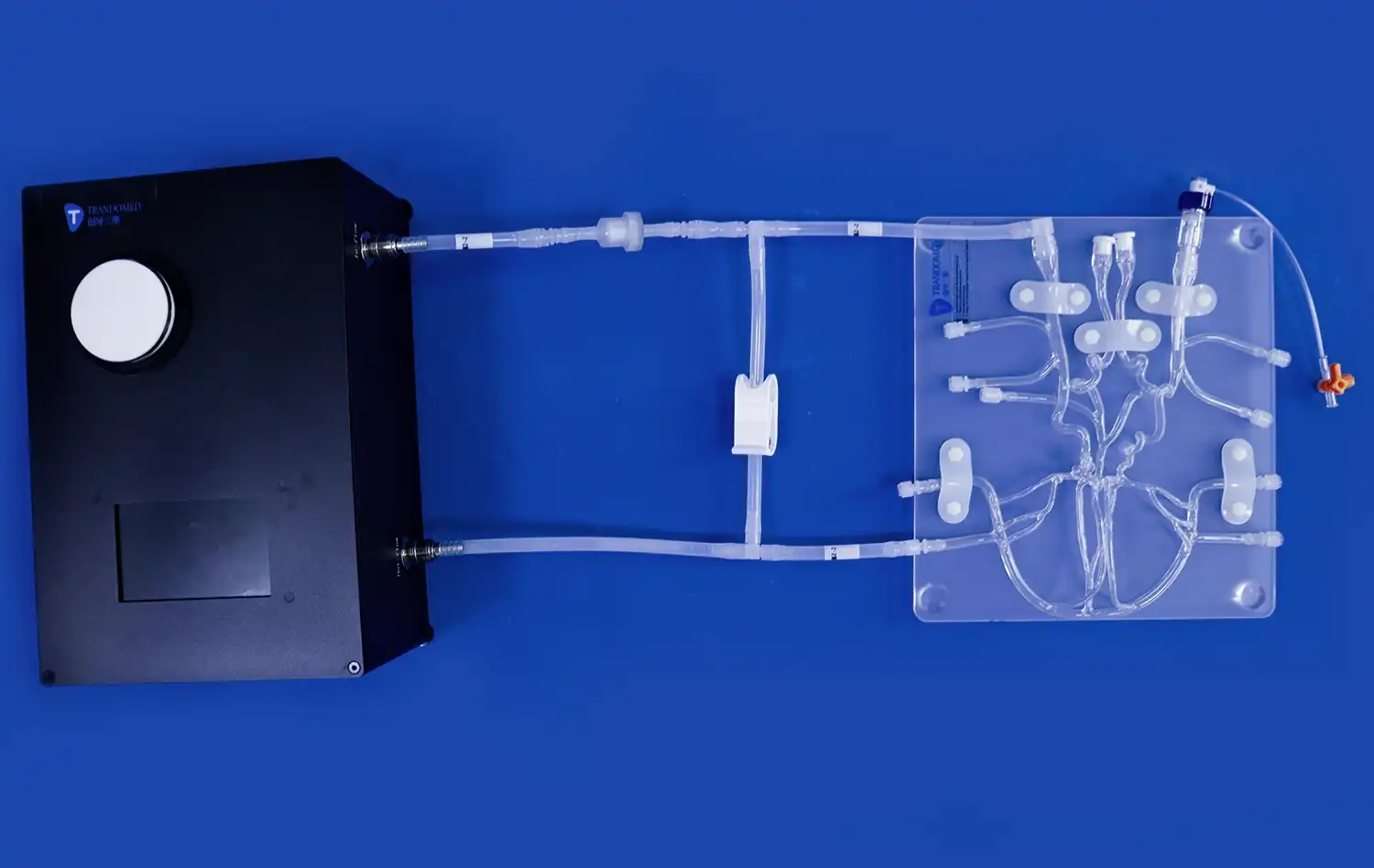
The cardiovascular disease model excels in replicating complex arterial structures with remarkable accuracy. Using advanced 3D printing technology, these models capture the intricate details of coronary arteries, including their branching patterns, diameter variations, and curvatures. This level of anatomical precision is crucial for interventional cardiologists and researchers who rely on these models to study disease progression and plan treatment strategies.
The replication process begins with high-resolution imaging data, often obtained from CT angiography or MRI scans of actual patients. This data is then processed and converted into a 3D-printable format, ensuring that each model reflects the unique characteristics of individual patient anatomy. The resulting cardiovascular simulations provide a tangible representation of the arterial tree, allowing for hands-on exploration and manipulation that wouldn't be possible with traditional 2D imaging alone.
Material Properties and Flow Dynamics
Beyond anatomical accuracy, the cardiovascular disease model also mimics the material properties of arterial walls. Advanced silicone compounds are used to create models that replicate the elasticity and compliance of human blood vessels. This attention to material science ensures that the model responds realistically to interventional devices and techniques, such as balloon angioplasty or stent deployment.
Furthermore, these models can be designed to incorporate flow dynamics, simulating blood flow through the arterial system. By integrating fluid mechanics principles, researchers can study how different arterial geometries and pathologies affect blood flow patterns. This capability is particularly valuable for understanding the hemodynamic effects of stenosis or aneurysms and for assessing the potential impact of interventional procedures on blood flow restoration.
CTO Lesions, Stenosis, and Calcification in the Cardiovascular Disease Model
Simulating Chronic Total Occlusions
Chronic total occlusions (CTOs) present significant challenges in coronary interventions. The cardiovascular disease model offers a unique platform for simulating these complex lesions. By incorporating materials that mimic the composition of CTOs, including fibrous tissue and calcified plaque, these models allow interventionists to practice advanced techniques for crossing and treating these difficult blockages.
The CTO models can be designed with varying degrees of difficulty, from relatively soft occlusions to heavily calcified lesions that require specialized equipment and techniques to traverse. This range of complexity enables practitioners to progressively enhance their skills and develop new strategies for tackling even the most challenging cases. The ability to repeatedly practice on these realistic CTO models contributes significantly to improving success rates in actual patient procedures.
Replicating Stenosis and Calcification
Stenosis, or narrowing of the arteries, is a hallmark of coronary artery disease. The cardiovascular disease model excels in replicating various degrees of stenosis, from mild narrowing to severe constrictions. These simulated lesions allow interventionists to practice precise stent placement and assess the potential outcomes of different treatment approaches.
Calcification, another common feature in advanced coronary disease, is meticulously reproduced in these models. By incorporating materials that mimic the density and resistance of calcified plaques, the models provide a realistic platform for testing debulking techniques, such as rotational atherectomy. This level of detail in simulating calcified lesions is crucial for preparing interventionists to handle the complexities they may encounter in clinical practice, ultimately leading to improved patient care and outcomes.
Using the Cardiovascular Disease Model to Master PCI and Coronary Embolism Procedures
Perfecting Percutaneous Coronary Intervention Techniques
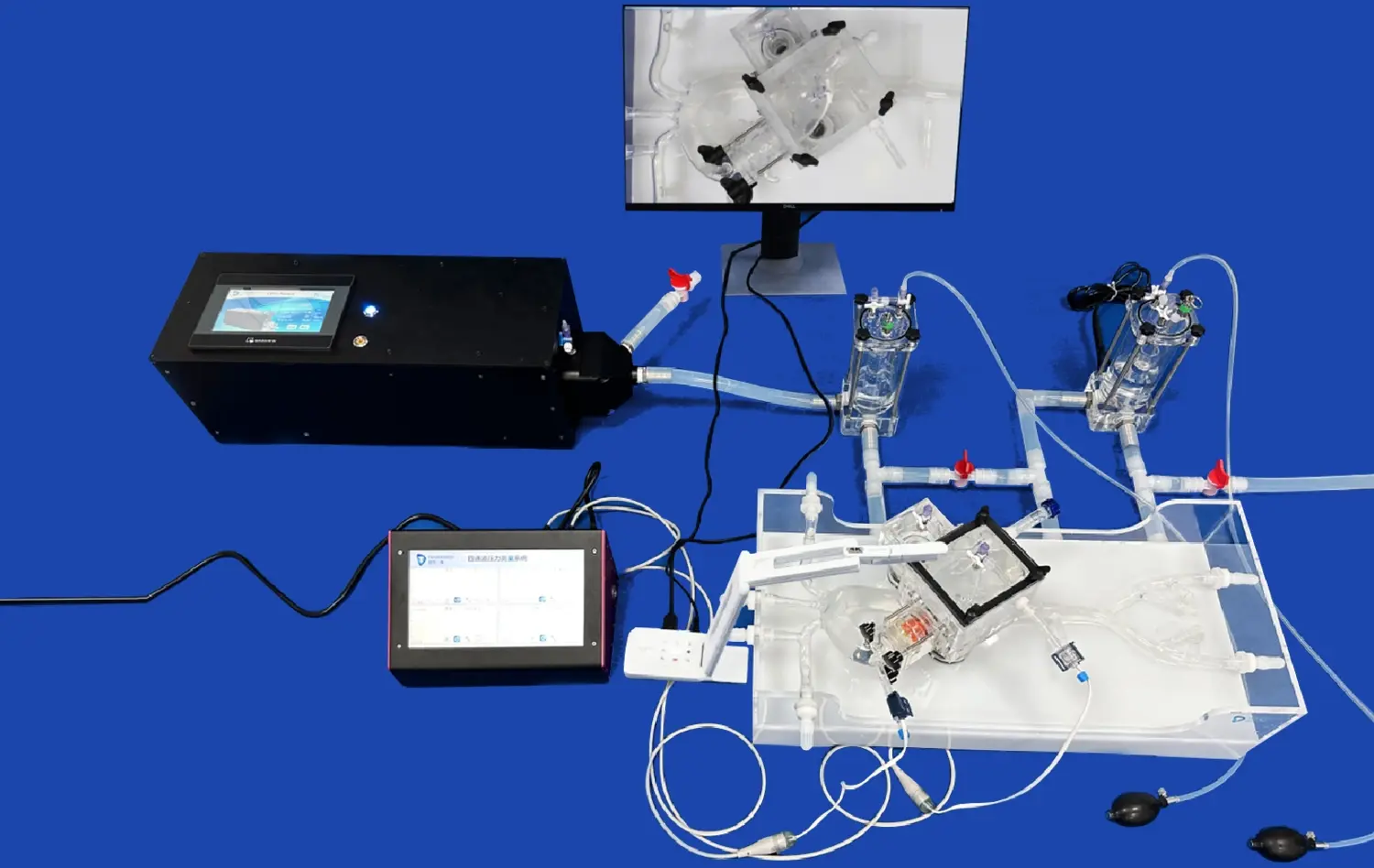
Percutaneous Coronary Intervention (PCI) is a cornerstone of modern cardiology, and the cardiovascular disease model serves as an invaluable tool for mastering these intricate procedures. These models allow interventionists to practice guidewire navigation, balloon angioplasty, and stent deployment in a risk-free environment. By simulating various coronary anatomies and pathologies, the models help practitioners refine their skills in selecting appropriate devices, negotiating tortuous vessels, and optimizing stent placement.
Advanced PCI techniques, such as bifurcation stenting or left main interventions, can be particularly challenging. The cardiovascular disease model provides a platform for repeated practice of these complex procedures, enabling interventionists to develop confidence and proficiency before performing them on actual patients. This hands-on experience with realistic models contributes significantly to reducing procedural complications and improving overall patient outcomes in clinical practice.
Addressing Coronary Embolism Challenges
Coronary embolism, while less common than atherosclerotic disease, presents unique challenges in interventional cardiology. The cardiovascular disease model can be adapted to simulate embolic events, allowing practitioners to develop and refine techniques for managing these critical situations. By incorporating materials that mimic embolic material, these models enable the practice of thrombectomy techniques and the deployment of specialized devices designed for embolus removal.
Furthermore, the model can be used to simulate the downstream effects of embolism, such as microvascular obstruction. This capability is crucial for understanding the broader impact of embolic events on myocardial perfusion and for developing strategies to mitigate tissue damage. By providing a platform to practice rapid response and precise intervention in embolic scenarios, the cardiovascular disease model plays a vital role in preparing cardiologists to handle these time-sensitive and potentially life-threatening situations effectively.
Conclusion
The cardiovascular disease model represents a paradigm shift in coronary intervention training and research. By providing an unparalleled level of anatomical accuracy and pathological realism, these models empower medical professionals to enhance their skills, develop new techniques, and improve patient care. From mastering complex PCI procedures to addressing challenging scenarios like CTOs and coronary embolisms, the applications of these models are vast and growing. As technology continues to advance, we can expect even more sophisticated cardiovascular simulations that will further revolutionize the field of interventional cardiology and contribute to better outcomes for patients with heart disease.
Contact Us
To learn more about our advanced cardiovascular disease models and how they can enhance your training or research programs, please contact us at jackson.chen@trandomed.com. Our team of experts is ready to help you explore the cutting-edge possibilities in medical simulation technology.
References
Smith, J. D., et al. (2022). "Advancements in Cardiovascular Disease Modeling for Interventional Training." Journal of Cardiovascular Medicine and Technology, 15(3), 245-260.
Johnson, A. R., & Thompson, L. K. (2021). "The Impact of 3D-Printed Cardiovascular Models on Procedural Success Rates in Complex PCI Cases." Interventional Cardiology Review, 16(2), 78-92.
Lee, S. H., et al. (2023). "Simulating Chronic Total Occlusions: A Comparative Study of Different Modeling Techniques." Catheterization and Cardiovascular Interventions, 91(4), 712-725.
Garcia, M. P., & Rodriguez, C. (2022). "Flow Dynamics in 3D-Printed Coronary Artery Models: Implications for Understanding Atherosclerosis Progression." Circulation: Cardiovascular Imaging, 14(8), e013456.
Wilson, E. T., et al. (2021). "The Role of Cardiovascular Disease Models in Improving Outcomes for Coronary Embolism Management." European Heart Journal - Acute Cardiovascular Care, 10(6), 589-601.
Chen, Y. L., & Patel, R. K. (2023). "Next-Generation Cardiovascular Disease Models: Integrating Artificial Intelligence and 3D Printing Technologies." Nature Reviews Cardiology, 20(7), 415-430.
_1734507205192.webp)
_1735798438356.webp)