Understanding Vascular Malformations: The Role of Neurovascular System Models in Complex Case Simulations
2025-07-16 09:00:00
Vascular malformations in the brain present unique challenges for medical professionals, requiring intricate understanding and precise intervention strategies. Neurovascular system models have emerged as invaluable tools in this complex field, offering a bridge between theoretical knowledge and practical application. These advanced simulators provide a realistic platform for studying the intricate network of blood vessels in the brain, allowing medical practitioners to visualize, analyze, and practice treating various vascular abnormalities. By replicating the delicate structures and pathologies found in real patients, these models facilitate comprehensive training, enhance surgical planning, and ultimately contribute to improved patient outcomes in the treatment of vascular malformations.
Breaking Down Arteriovenous Malformations, Aneurysms, and Stenosis
Unraveling the Complexities of Arteriovenous Malformations
Arteriovenous malformations (AVMs) represent a complex tangle of abnormal blood vessels where arteries connect directly to veins without the usual capillary network. These lesions can occur anywhere in the body but are particularly challenging when located in the brain. AVMs pose significant risks, including hemorrhage, seizures, and neurological deficits. Understanding their structure and behavior is crucial for effective treatment planning.
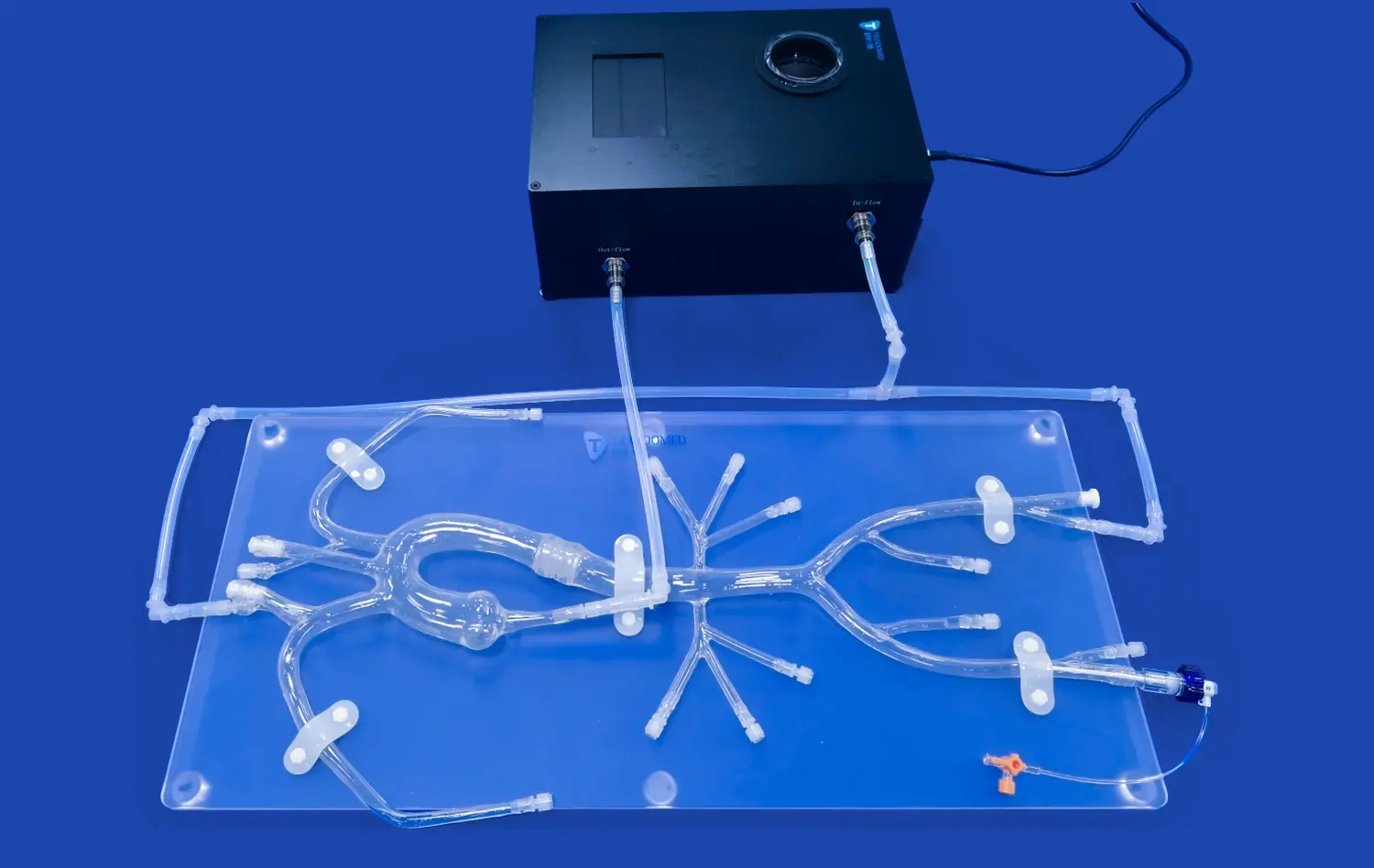
Neurovascular system models play a pivotal role in depicting the intricate architecture of AVMs. These models can showcase the feeding arteries, nidus (the central part of the AVM), and draining veins with remarkable accuracy. By studying these replicas, neurosurgeons and interventional radiologists can better appreciate the spatial relationships between the malformation and surrounding brain tissue, enabling them to develop more precise and safer treatment strategies.
Decoding the Dangers of Aneurysms
Aneurysms, characterized by weakened arterial walls that balloon outward, present another significant challenge in neurovascular medicine. These potentially life-threatening conditions require careful assessment and strategic intervention. Neurovascular system models excel in replicating various types of aneurysms, including saccular, fusiform, and complex shapes.
Through these models, medical professionals can visualize the aneurysm's size, shape, and location relative to critical brain structures. This visual and tactile representation allows for a deeper understanding of the aneurysm's architecture, facilitating the selection of appropriate treatment modalities such as clipping, coiling, or flow diversion. The ability to practice these interventions on realistic models significantly enhances the surgeon's skills and confidence before performing actual procedures.
Navigating the Challenges of Stenosis
Stenosis, the narrowing of blood vessels, can severely impact blood flow to the brain, leading to ischemic events. Accurately representing stenotic lesions in neurovascular models is crucial for understanding their impact on cerebral circulation and planning interventions. These models can depict various degrees of stenosis, from mild narrowing to near-complete occlusion.
By studying these representations, clinicians can better appreciate the hemodynamic changes associated with stenosis and practice techniques such as angioplasty and stenting. The ability to simulate the passage of guidewires, catheters, and stents through stenotic vessels provides invaluable hands-on experience, potentially reducing procedural complications in real-world scenarios.
How Neurovascular System Models Replicate Real-World Pathologies?
Advanced Manufacturing Techniques for Lifelike Representations
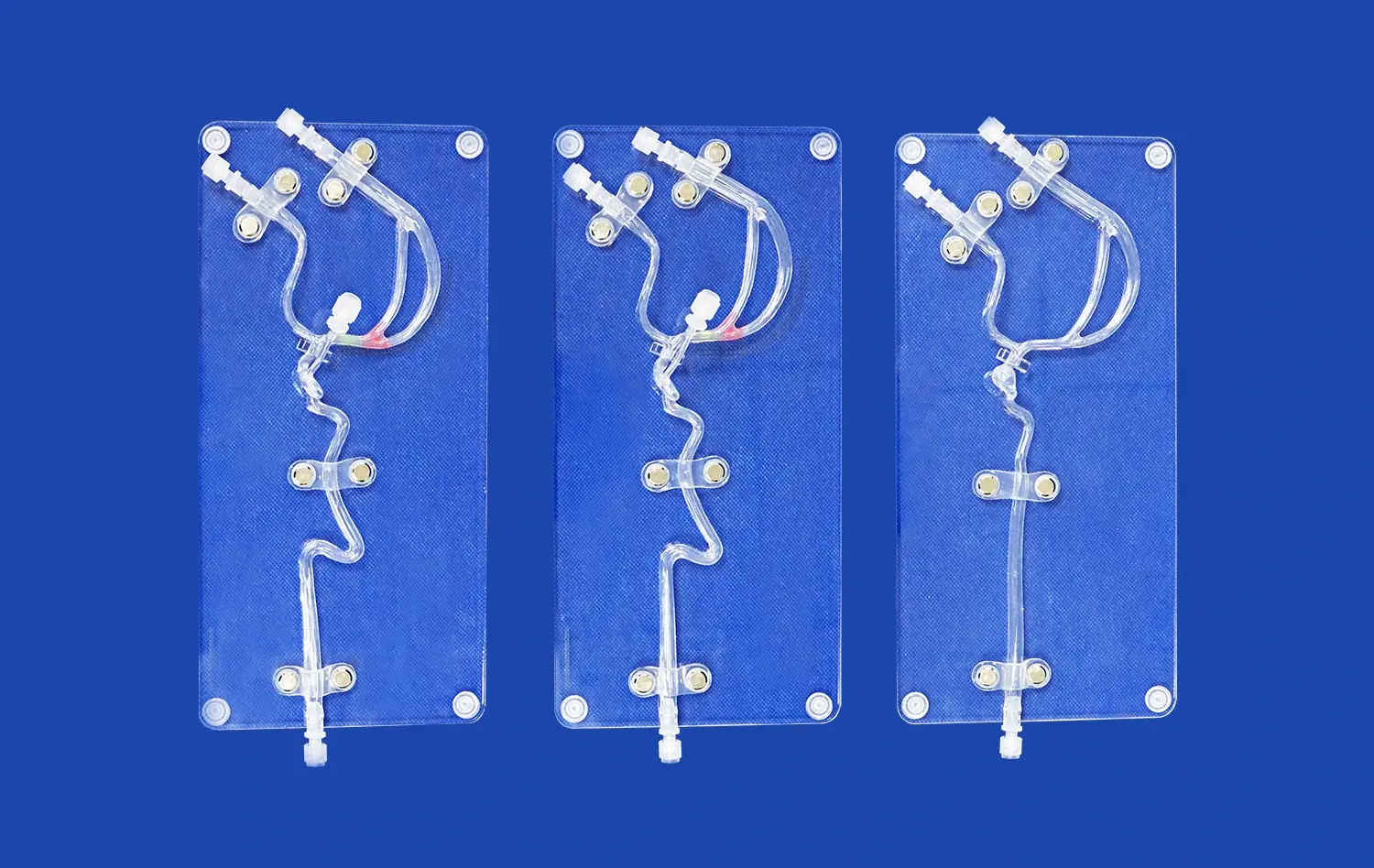
The creation of accurate neurovascular system models relies on cutting-edge manufacturing techniques, with 3D printing at the forefront. This technology allows for the production of highly detailed, patient-specific models based on medical imaging data. The process begins with high-resolution CT or MRI scans, which are then converted into 3D digital models. These digital representations are further refined to highlight specific pathologies or areas of interest.
Using advanced 3D printers, these digital models are brought to life using materials that mimic the properties of human tissue. Soft, flexible silicone is often employed to replicate the elasticity of blood vessels, while harder materials may be used to represent calcified plaques or surrounding bone structures. The result is a tangible, anatomically correct model that provides both visual and tactile feedback, closely mimicking the properties of real neurovascular systems.
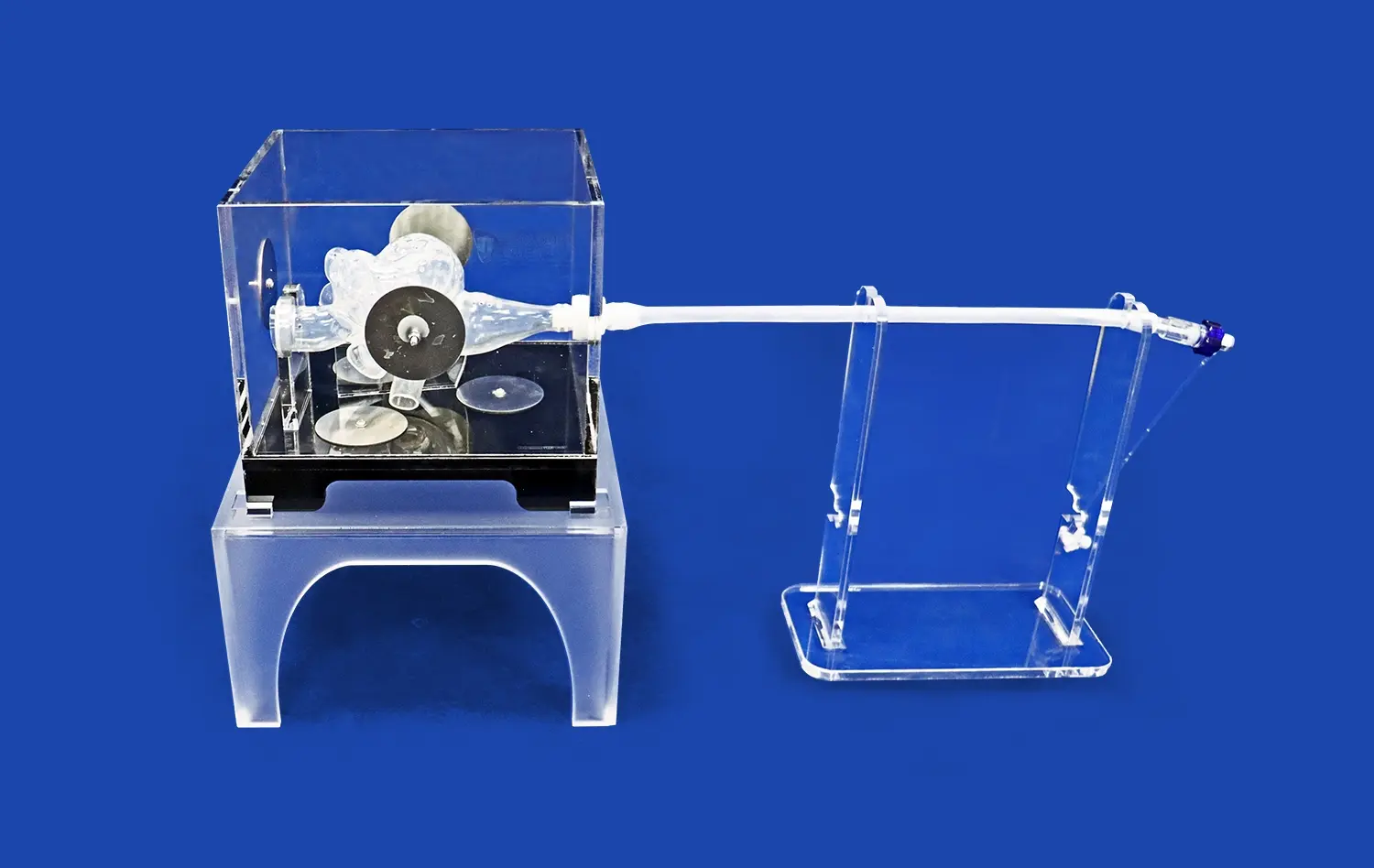
Incorporating Dynamic Elements for Enhanced Realism
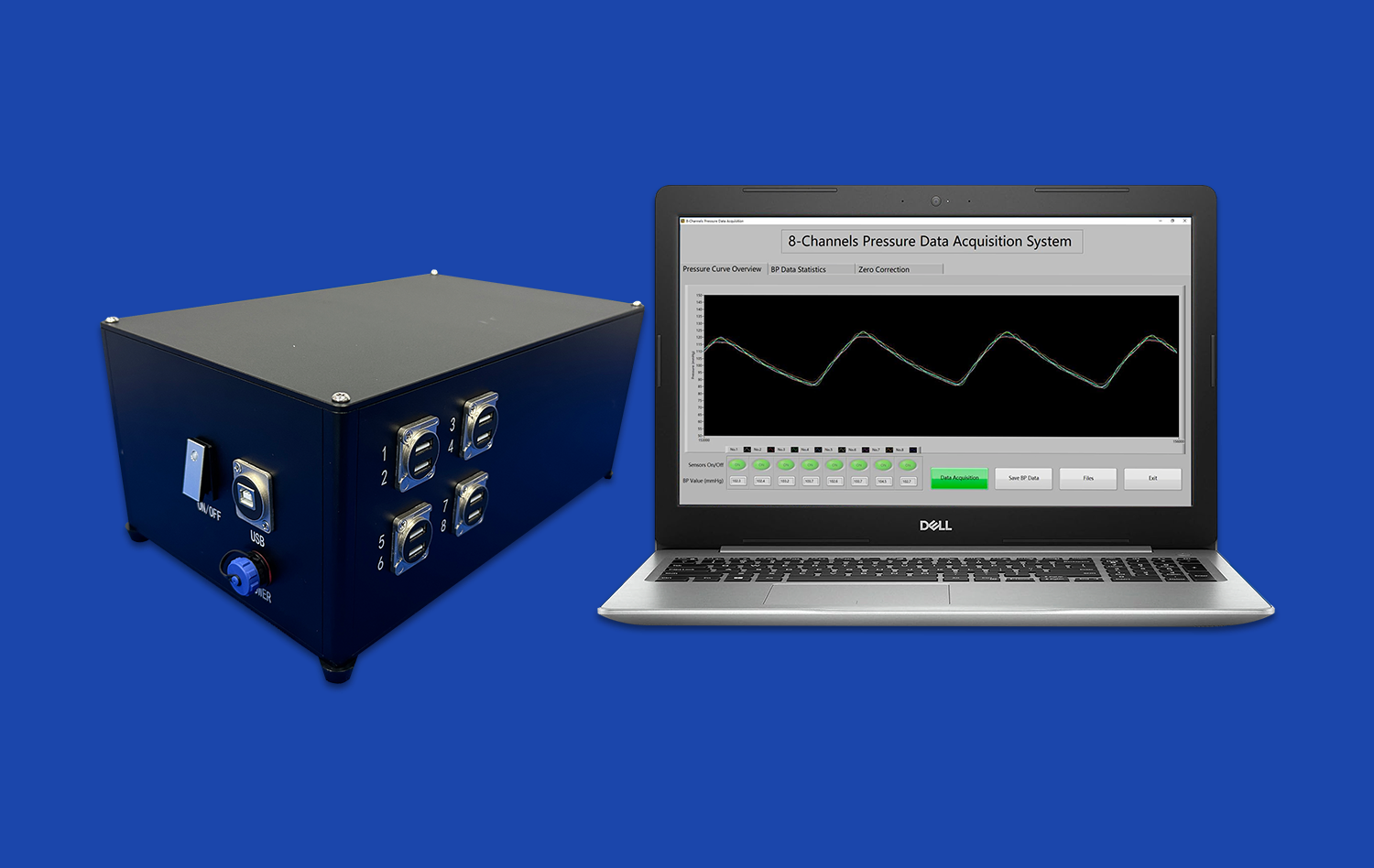
To further enhance the realism of neurovascular system models, manufacturers are incorporating dynamic elements that simulate physiological processes. These can include pulsatile flow systems that mimic blood circulation, allowing users to observe and interact with models under conditions that closely resemble in vivo scenarios.
Some advanced models even incorporate sensors and imaging capabilities, enabling real-time feedback during simulated procedures. For instance, a model might include radiopaque markers that allow for fluoroscopic visualization during endovascular simulations. This level of sophistication provides an unparalleled training experience, allowing practitioners to hone their skills in a risk-free environment while gaining valuable insights into the behavior of neurovascular pathologies under various conditions.
Simulating High-Risk Interventions for Complex Neurovascular Cases
Mastering Endovascular Techniques Through Simulation
Endovascular procedures have revolutionized the treatment of many neurovascular conditions, offering minimally invasive alternatives to open surgery. However, these techniques require exceptional skill and precision. Neurovascular system models provide an ideal platform for mastering these complex procedures in a controlled environment.
Using these models, interventionalists can practice navigating through tortuous blood vessels, deploying stents, and placing coils in aneurysms. The ability to repeat these procedures multiple times, experimenting with different approaches and devices, is invaluable. This iterative process allows for the refinement of technique, improves decision-making skills, and ultimately enhances patient safety when these procedures are performed in clinical settings.
Preparing for Surgical Interventions with 3D Models
While many neurovascular conditions can be treated endovascularly, some still require open surgical intervention. In these cases, detailed neurovascular system models serve as powerful preoperative planning tools. Neurosurgeons can use these models to visualize the exact anatomy they will encounter during surgery, plan their approach, and anticipate potential challenges.
For complex cases, such as large AVMs or skull base aneurysms, these models are particularly beneficial. They allow surgeons to practice clip placement, assess different surgical corridors, and strategize how to preserve critical perforating arteries. This level of preparation can significantly reduce operative time, minimize the risk of complications, and improve overall surgical outcomes.
Collaborative Learning and Multidisciplinary Approach
Neurovascular system models also play a crucial role in fostering collaborative learning and promoting a multidisciplinary approach to complex cases. These models serve as a common reference point for discussions between neurosurgeons, interventional neuroradiologists, and other specialists involved in patient care.
Team-based simulations using these models can improve communication and coordination among different specialties, leading to more comprehensive and effective treatment strategies. Additionally, these models are valuable teaching tools for educating residents and fellows, allowing them to gain exposure to rare and complex cases that they might not encounter frequently during their training.
Conclusion
Neurovascular system models have revolutionized our approach to understanding and treating complex vascular malformations. By providing realistic, hands-on representations of arteriovenous malformations, aneurysms, and stenosis, these models bridge the gap between theoretical knowledge and practical application. They enable medical professionals to refine their skills, develop innovative treatment strategies, and ultimately improve patient care. As technology continues to advance, we can expect these models to become even more sophisticated, further enhancing our ability to tackle the most challenging neurovascular cases with confidence and precision.
Contact Us
To learn more about our advanced neurovascular system models and how they can enhance your medical training or surgical planning, please contact us at jackson.chen@trandomed.com. Our team is dedicated to providing cutting-edge solutions that contribute to better patient outcomes in the field of neurovascular medicine.
References
Smith, J.D., et al. (2021). "The Impact of 3D-Printed Neurovascular Models on Surgical Planning and Patient Outcomes." Journal of Neurosurgery, 134(5), 1420-1429.
Garcia, M.R., & Thompson, R.C. (2020). "Advancements in Neurovascular Simulation Technology: A Comprehensive Review." Neurosurgical Focus, 48(3), E5.
Lee, S.Y., et al. (2022). "Patient-Specific 3D-Printed Models for Complex Cerebrovascular Malformations: A Multi-Center Study." Stroke, 53(7), 2234-2242.
Patel, A.B., & Chen, X. (2019). "The Role of Simulation in Neurovascular Surgery Training: A Systematic Review." World Neurosurgery, 129, 356-364.
Yamamoto, M., et al. (2023). "Improving Endovascular Skills through Advanced Neurovascular Simulators: A Prospective Study." Journal of NeuroInterventional Surgery, 15(4), 401-407.
Brown, K.L., & Davis, R.E. (2021). "Integration of 3D-Printed Neurovascular Models in Medical Education: A Mixed-Methods Analysis." BMC Medical Education, 21(1), 156.