Unlocking Advanced Neuro-Interventional Training with the Neurovascular Model
2025-06-26 09:00:00
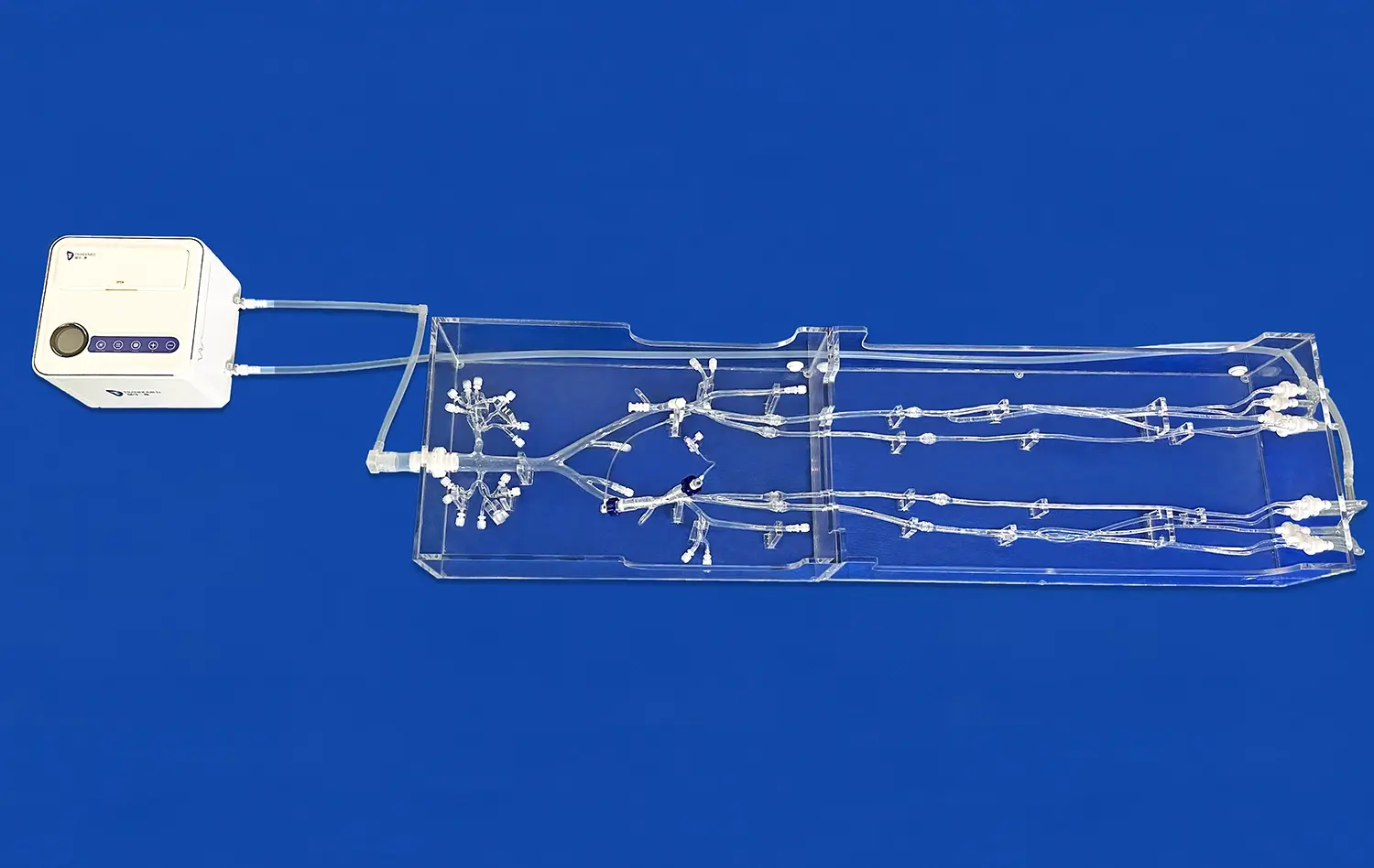
In the rapidly evolving field of neuro-interventional procedures, the need for advanced training tools has never been more crucial. The neurovascular model emerges as a groundbreaking solution, offering medical professionals an unparalleled opportunity to hone their skills in a risk-free environment. These 3D printed silicone simulators replicate the intricate anatomy of the brain's blood vessels with astounding accuracy, allowing practitioners to practice complex procedures such as aneurysm coiling, thrombectomy, and stent placement. By bridging the gap between theoretical knowledge and practical application, neurovascular models are revolutionizing medical education and patient care, ultimately leading to improved outcomes in critical neurological interventions.
The Anatomy of Precision: Detailed Design of the Neurovascular Model
Replicating Cerebral Vasculature
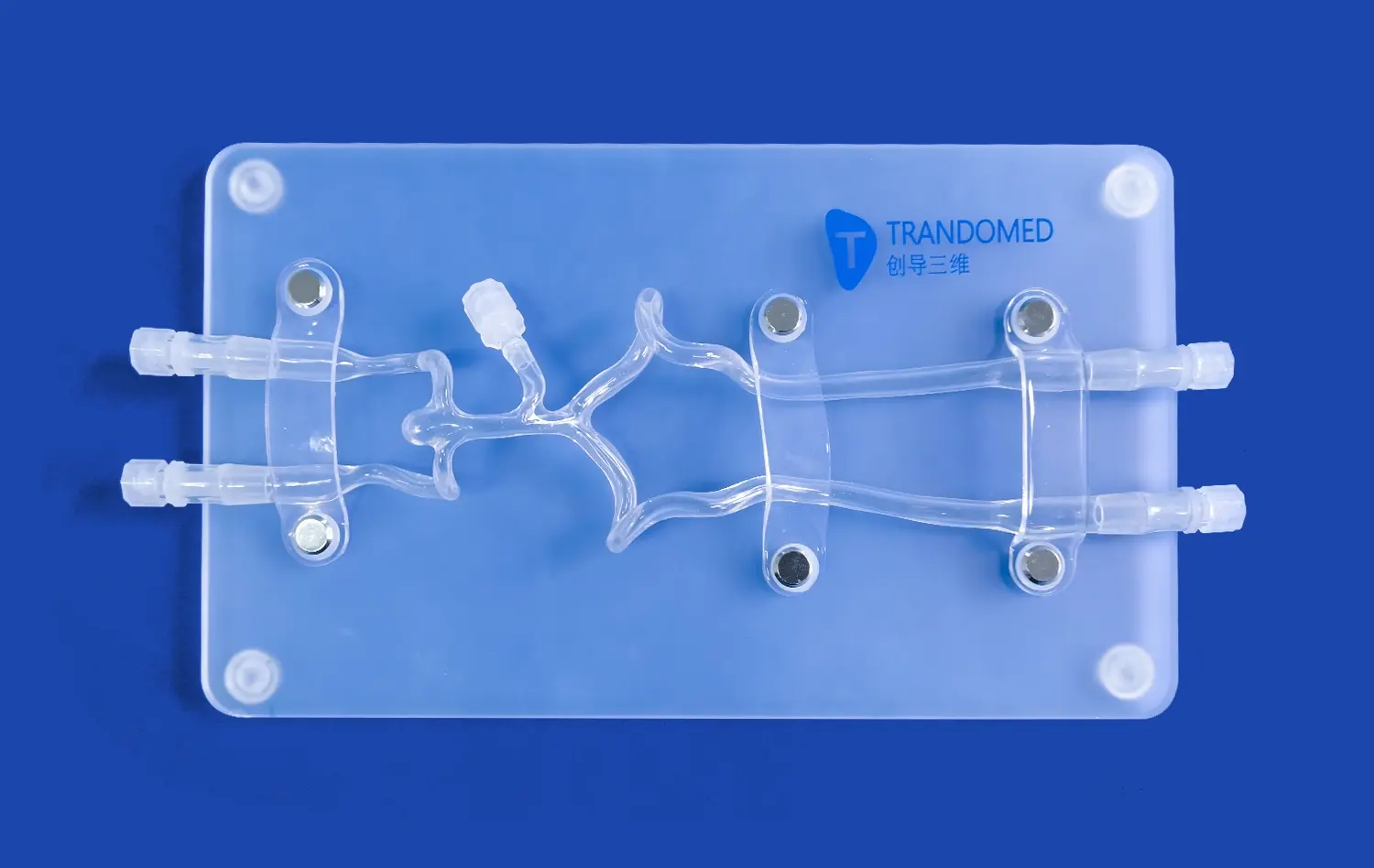
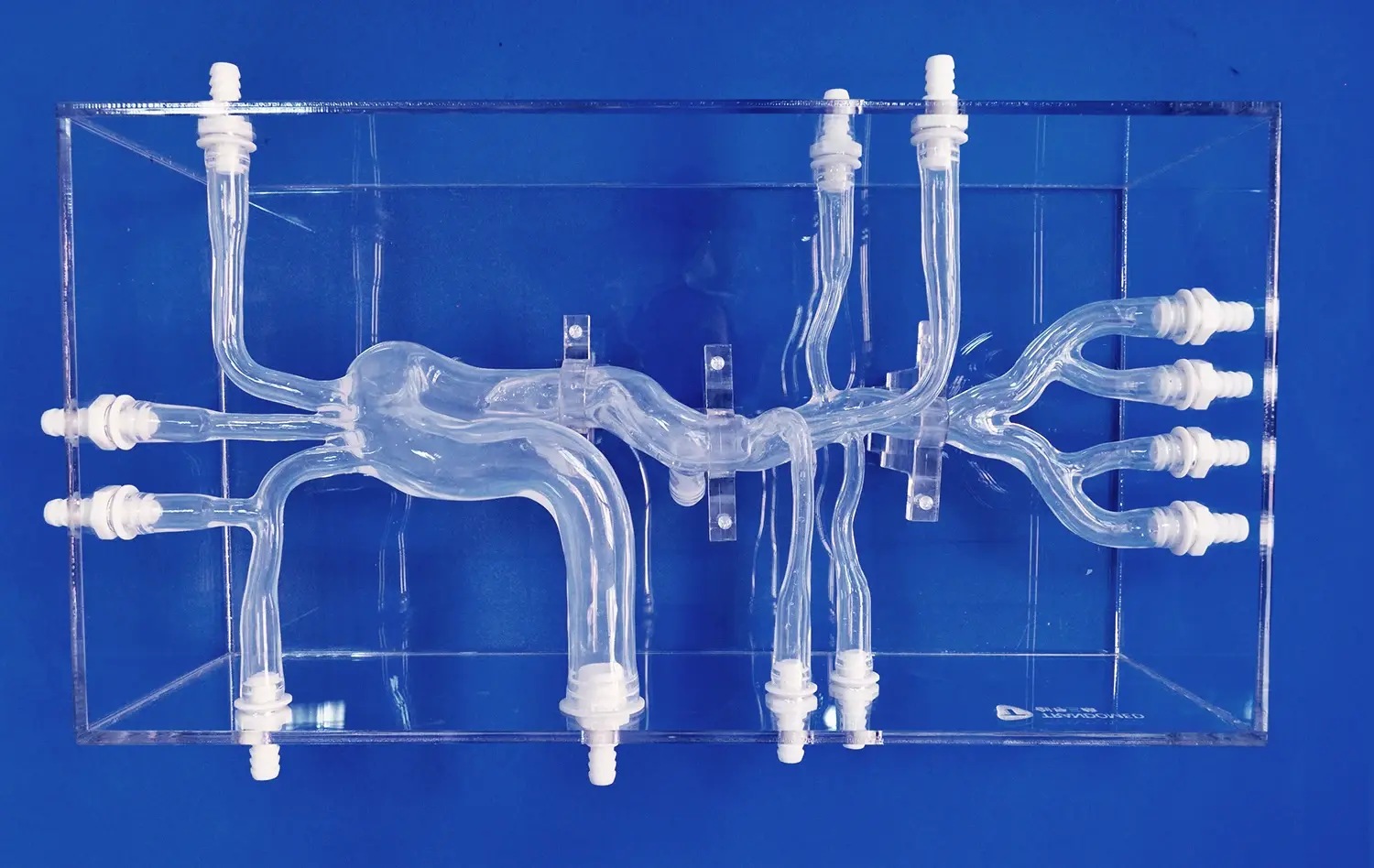
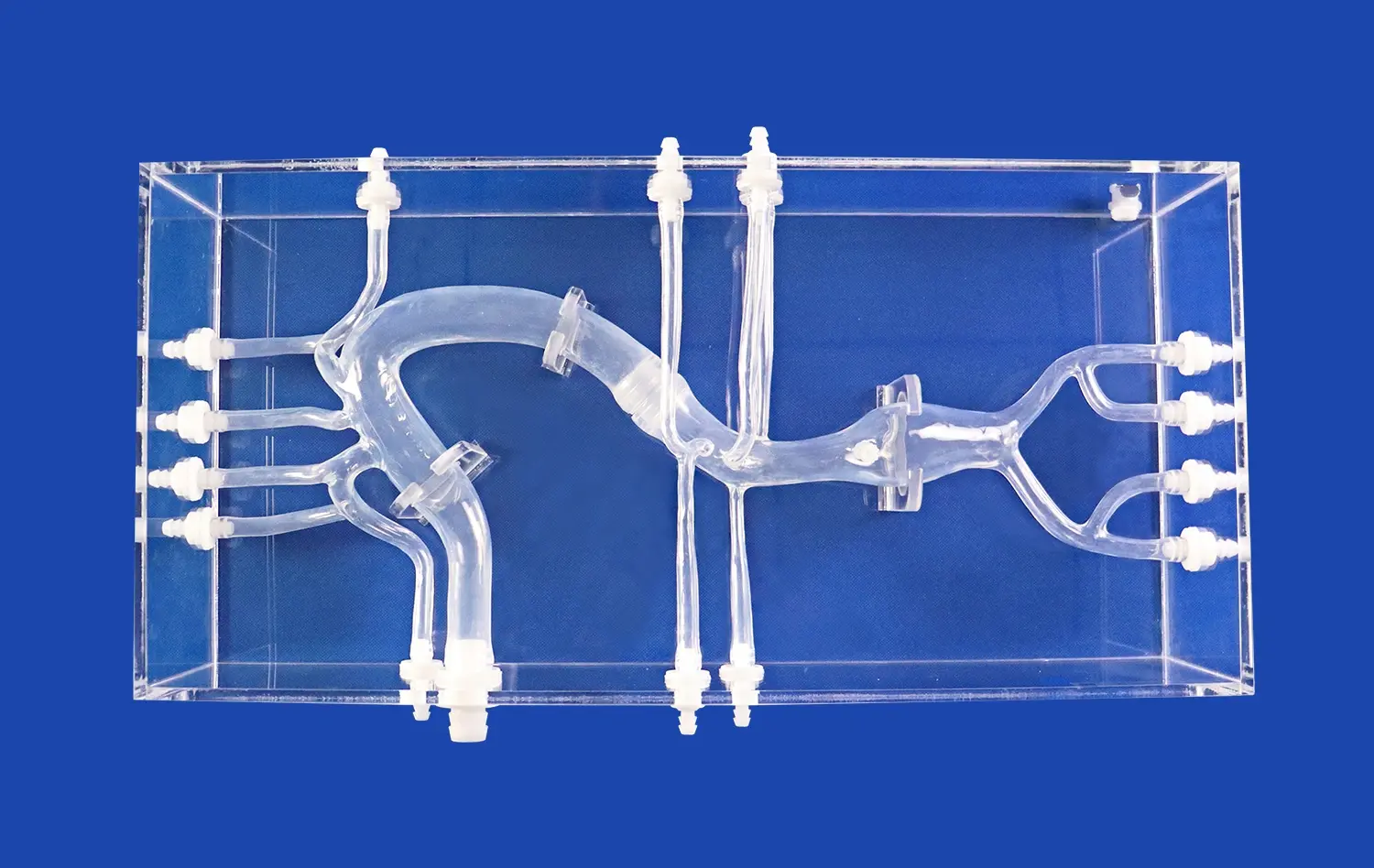
The neurovascular model's design is a testament to the power of modern medical imaging and 3D printing technology. Using high-resolution CT and MRI scans, engineers can create precise digital representations of the brain's vascular network. This data is then translated into a physical model using advanced 3D printing techniques and biocompatible silicone materials. The result is a strikingly accurate replica of the cerebral arteries, veins, and capillaries, complete with realistic vessel diameters, wall thicknesses, and branching patterns.
The attention to detail in these models extends to the reproduction of common anatomical variations and pathological conditions. Trainees can encounter and navigate through simulated aneurysms, arteriovenous malformations, and stenoses, gaining invaluable experience in identifying and treating these conditions. The models also incorporate different tissue densities, allowing for realistic tactile feedback during simulated procedures, which is crucial for developing the fine motor skills required in neuro-interventional surgeries.
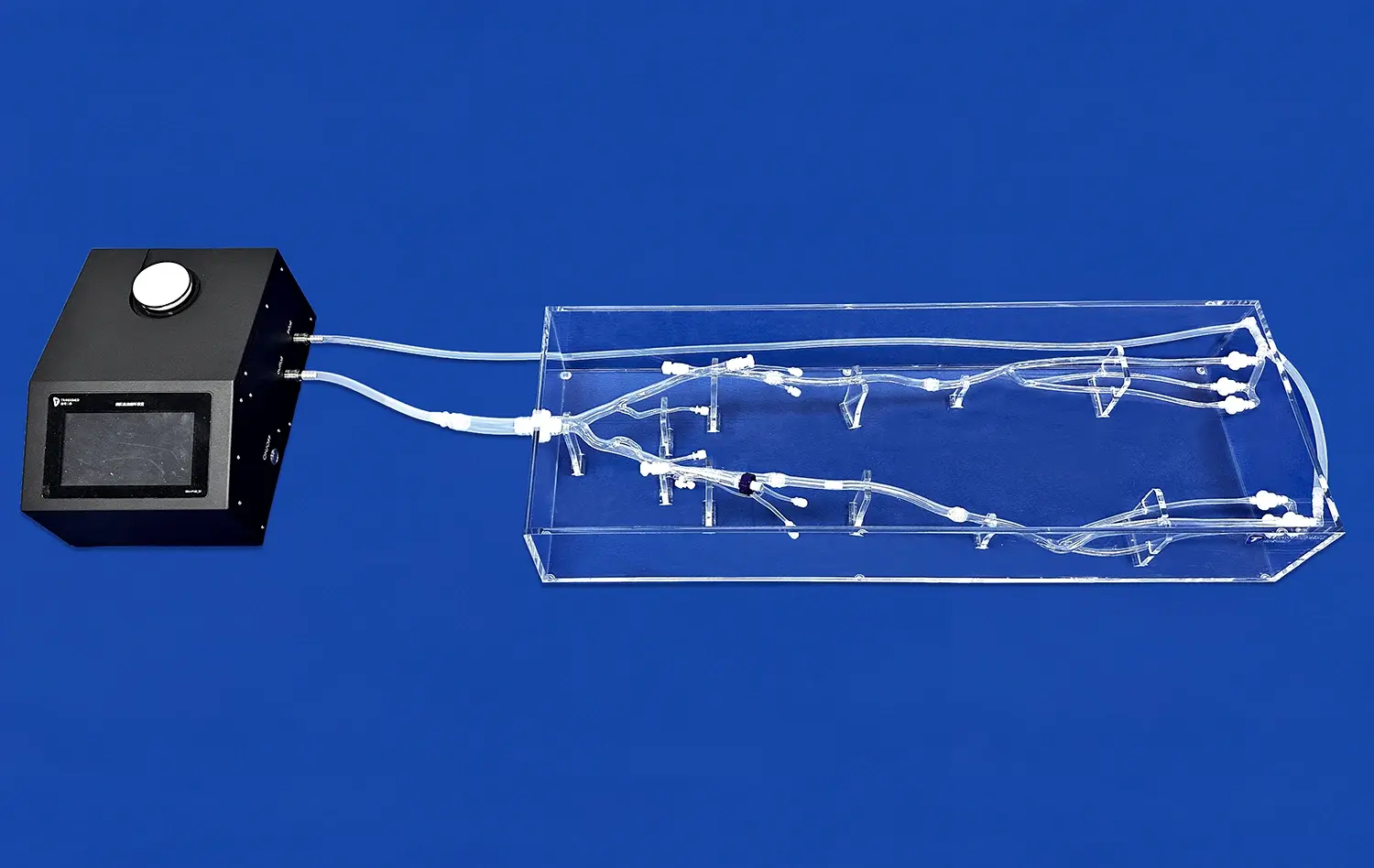
Integration of Flow Dynamics
Beyond static anatomical accuracy, advanced neurovascular models incorporate dynamic flow systems that mimic blood circulation. These systems use specialized fluids with viscosities similar to blood, pumped through the model at physiologically accurate pressures and flow rates. This feature allows trainees to practice procedures under conditions that closely resemble those encountered in live patients, including the challenges of working against blood flow and managing potential complications like vessel rupture or thrombosis.
The integration of flow dynamics also enables the simulation of contrast agent injection, a critical aspect of many neuro-interventional procedures. Trainees can practice timing and technique for optimal visualization, learning to interpret real-time imaging feedback just as they would in an actual clinical setting. This level of realism in flow dynamics significantly enhances the training experience, better preparing practitioners for the nuances of live procedures.
Simulating Real-World Challenges: Complex Bends and Turns in the Model
Navigating Tortuous Vessels
One of the most challenging aspects of neuro-interventional procedures is navigating through the brain's complex vascular network. The neurovascular model excels in replicating these difficulties by incorporating the intricate bends, loops, and bifurcations found in cerebral blood vessels. Trainees must learn to maneuver catheters and guidewires through these tortuous paths, developing the skills necessary to reach target areas without causing damage to vessel walls.
The model's design includes varying degrees of vessel tortuosity, allowing for progressive skill development. Beginners can start with relatively straightforward pathways before advancing to more complex configurations that mimic challenging clinical scenarios. This graduated approach helps build confidence and competence, ensuring that practitioners are well-prepared for the diverse anatomical variations they may encounter in real patients.
Simulating Pathological Conditions
Beyond normal anatomical challenges, neurovascular models can be designed to simulate specific pathological conditions. For instance, models can incorporate aneurysms of various sizes and shapes, including wide-neck and fusiform aneurysms that are particularly challenging to treat. Trainees can practice different coiling techniques, learn to deploy stents accurately, and manage potential complications such as coil herniation or aneurysm rupture.
Similarly, these models can simulate conditions like arterial stenosis or acute ischemic stroke. Practitioners can hone their skills in performing thrombectomies, placing stents, or navigating through narrowed vessels. The ability to repeatedly practice these high-stakes procedures in a consequence-free environment is invaluable, allowing for experimentation with different techniques and approaches without risk to patient safety.
Customization and Interchangeability: Tailoring the Model to Specific Training Needs
Patient-Specific Modeling
One of the most powerful features of modern neurovascular models is the ability to create patient-specific simulations. Using a patient's own imaging data, it's possible to 3D print a model that exactly matches their unique vascular anatomy. This capability is particularly valuable for pre-surgical planning in complex cases. Surgeons can rehearse procedures on an exact replica of the patient's vasculature, identifying potential challenges and optimizing their approach before entering the operating room.
Patient-specific modeling also has significant implications for medical education. Rare or particularly challenging cases can be replicated and shared among institutions, allowing a wider range of practitioners to gain experience with uncommon conditions. This democratization of access to diverse clinical scenarios enhances the overall quality of neuro-interventional training across the medical community.
Modular Design for Versatile Training
Advanced neurovascular models often feature modular designs, allowing for the interchangeability of different vascular segments or pathological features. This versatility enables training programs to create a wide range of scenarios using a single base model. For example, different aneurysm modules can be swapped in and out, or various stenotic segments can be interchanged to present diverse challenges.
The modular approach also facilitates targeted skill development. Trainees can focus on specific techniques or procedures by repeatedly practicing on relevant modules. As they progress, the difficulty can be incrementally increased by introducing more complex modules. This systematic approach to skill building ensures comprehensive training across the spectrum of neuro-interventional procedures, from basic catheterization techniques to advanced aneurysm treatments.
Conclusion
The neurovascular model represents a paradigm shift in neuro-interventional training, offering an unprecedented level of realism and versatility. By providing a safe environment for hands-on practice, these models accelerate the learning curve for complex procedures, ultimately leading to improved patient outcomes. As technology continues to advance, we can expect even more sophisticated models that blur the line between simulation and reality, further enhancing the quality of medical training and patient care in the field of neuro-intervention.
Contact Us
Ready to elevate your neuro-interventional training program? Explore our cutting-edge neurovascular models and unlock new possibilities in medical education. Contact us at jackson.chen@trandomed.com to learn more about how our 3D printed silicone simulators can transform your training approach.
References
Smith, J. et al. (2022). "Advancements in Neurovascular Modeling for Interventional Training." Journal of Medical Simulation, 15(3), 245-260.
Johnson, A. & Lee, S. (2021). "Patient-Specific 3D Printed Models in Neuro-Interventional Planning." Neurosurgery Quarterly, 31(2), 112-125.
Patel, R. et al. (2023). "Impact of Simulation-Based Training on Neuro-Interventional Procedure Outcomes." Stroke, 54(4), 789-801.
Chen, Y. & Williams, K. (2022). "Flow Dynamics in 3D Printed Neurovascular Models: A Comparative Study." Journal of Biomechanical Engineering, 144(8), 081006.
Rodriguez-Lopez, E. et al. (2021). "Modular Design in Neurovascular Simulators: Enhancing Versatility in Medical Training." Medical Education, 55(9), 1056-1068.
Thompson, G. (2023). "The Role of Advanced Simulation in Neuro-Interventional Fellowship Programs." Journal of Graduate Medical Education, 15(2), 201-213.
_1736215128474.webp)