Why Are Anatomical Models Critical for Endovascular Training?
Enhancing Procedural Proficiency
Anatomical models play a crucial role in endovascular training by providing a tangible, three-dimensional representation of the vascular system. Unlike traditional learning methods that rely on textbooks or two-dimensional images, these models allow trainees to interact with a realistic replica of the human anatomy. This hands-on approach significantly enhances procedural proficiency by enabling practitioners to develop muscle memory and spatial awareness essential for performing complex endovascular procedures.
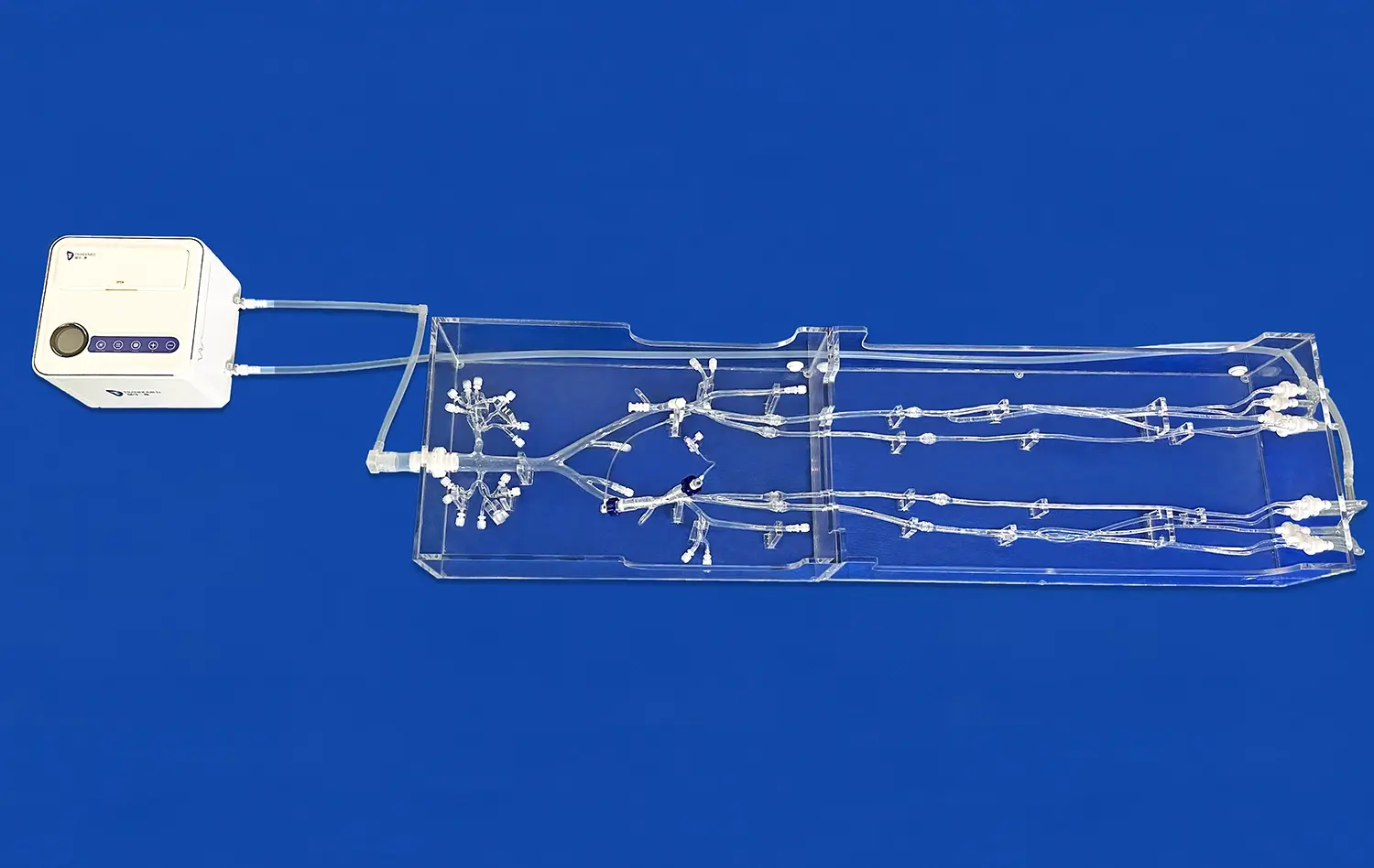
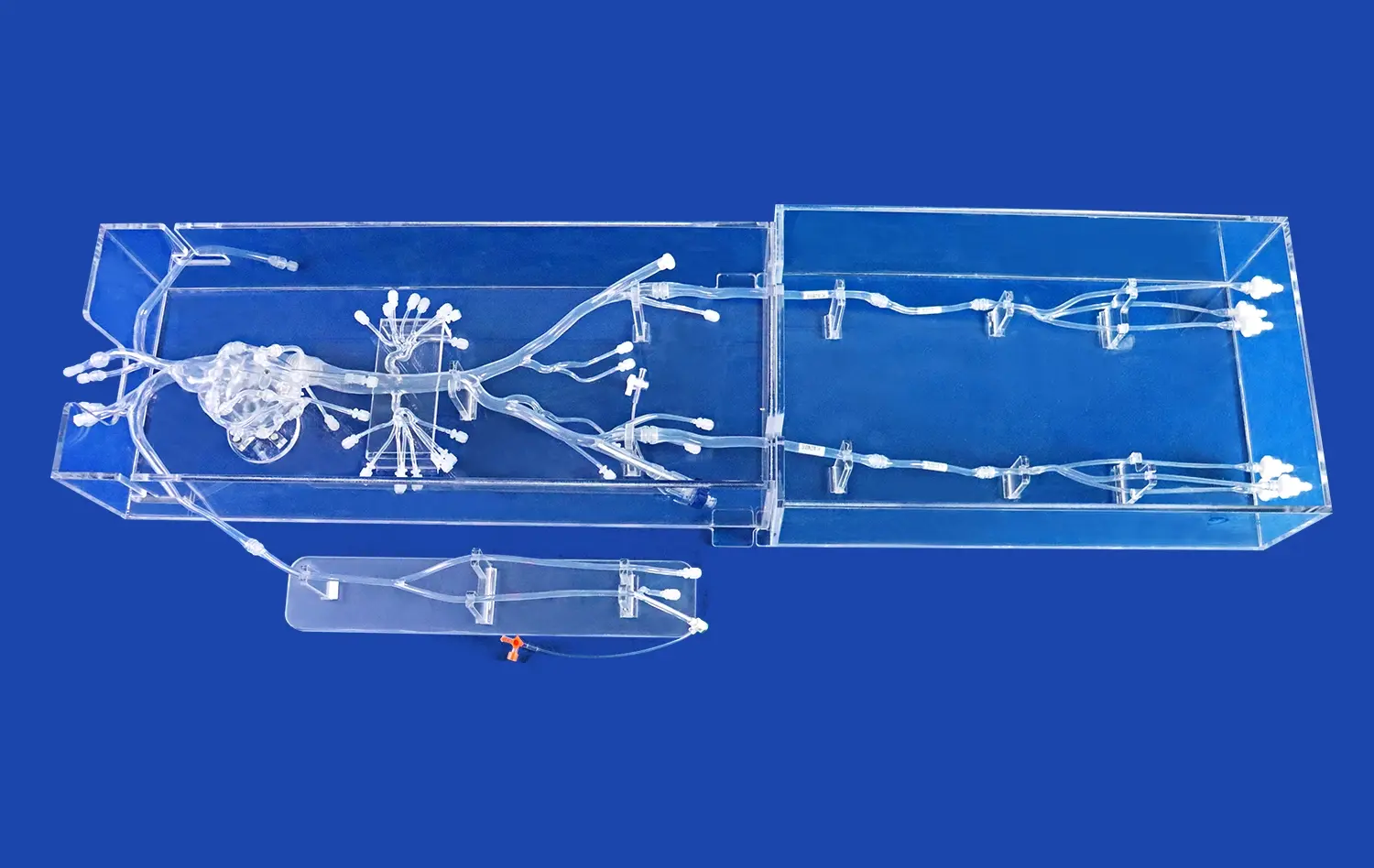
The Leg Arteries Model, for instance, offers a true-to-life representation of the lower limb vasculature, complete with accurate vessel diameters, branching patterns, and anatomical landmarks. This level of detail allows trainees to practice navigating through the arterial network, understanding the challenges posed by tortuous vessels, and developing strategies to overcome anatomical variations they may encounter in real patients.
Bridging the Gap Between Theory and Practice
Anatomical models serve as a crucial bridge between theoretical knowledge and practical application in endovascular training. While textbooks and lectures provide the foundational understanding of vascular anatomy and pathology, models offer the opportunity to apply this knowledge in a practical setting. This transition is vital for developing the confidence and competence necessary to perform procedures on actual patients.
By using models like the leg arteries model, trainees can visualize complex anatomical relationships, understand the three-dimensional orientation of vessels, and practice decision-making in various clinical scenarios. This experiential learning reinforces theoretical concepts and helps trainees develop a more intuitive understanding of endovascular procedures.
Facilitating Standardized Training and Assessment
Anatomical models provide a standardized platform for training and assessment in endovascular procedures. Unlike cadavers or animal models, which can vary significantly in anatomy and pathology, synthetic models offer consistent and reproducible learning experiences. This standardization is crucial for developing uniform training protocols and objective assessment criteria across medical institutions.
The Leg Arteries Model, with its modular design and customizable pathologies, allows educators to create specific training scenarios tailored to different skill levels and learning objectives. This flexibility enables the implementation of structured training programs that systematically build competence in endovascular techniques, from basic wire and catheter manipulation to complex interventions for peripheral artery disease.
Simulating Retrograde and Antegrade Access Techniques
Mastering Retrograde Access
Retrograde access is a fundamental technique in endovascular procedures, particularly for treating lesions in the lower extremities. The Leg Arteries Model excels in simulating this approach, allowing practitioners to perfect their skills in accessing the arterial system from a distal entry point and navigating towards the heart. This technique is crucial for crossing chronic total occlusions or treating lesions that are difficult to approach from an antegrade direction.
Using the model, trainees can practice inserting guidewires and catheters through the posterior tibial or dorsalis pedis arteries, navigating through the popliteal and femoral arteries, and reaching target lesions in the superficial femoral or iliac arteries. The model's realistic vessel compliance and accurate representation of anatomical curves provide authentic tactile feedback, helping trainees develop the finesse required for successful retrograde procedures.
Perfecting Antegrade Access
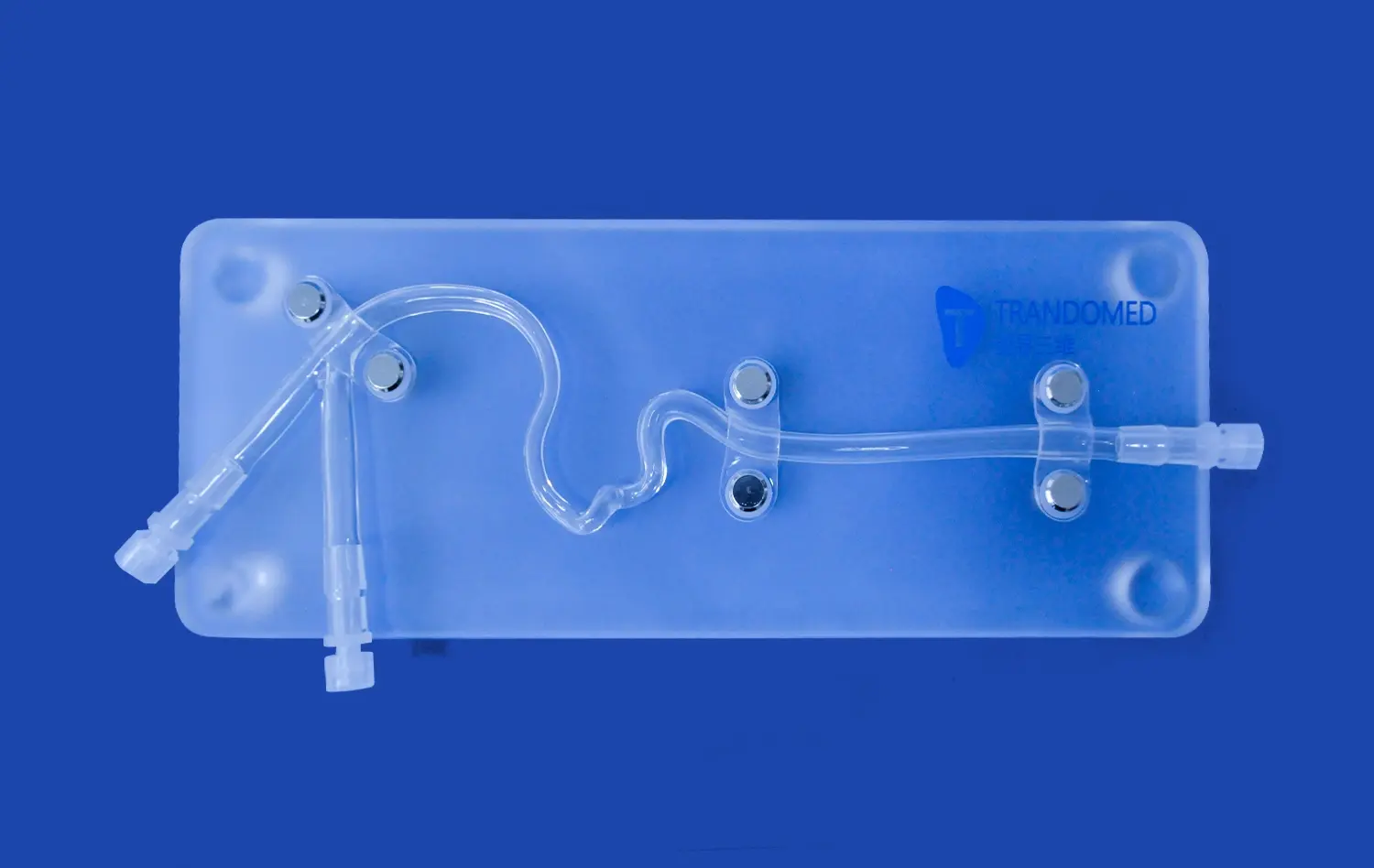
Antegrade access, typically performed through the common femoral artery, is the most common approach for lower extremity endovascular interventions. The leg arteries modeloffers multiple access points that simulate the common femoral artery, allowing trainees to practice this critical technique under various conditions.
Practitioners can hone their skills in needle puncture, wire insertion, and sheath placement – all crucial steps in establishing safe and effective arterial access. The model's design incorporates realistic tissue resistance and vessel wall properties, providing authentic tactile feedback during these maneuvers. This fidelity helps trainees develop the sensitivity and precision needed to avoid complications such as dissection or hematoma formation during real procedures.
Combining Access Techniques for Complex Interventions
Advanced endovascular procedures often require a combination of retrograde and antegrade access techniques. The Leg Arteries Model's versatility shines in simulating these complex scenarios, allowing practitioners to practice coordinated dual-access approaches. This capability is particularly valuable for treating long chronic total occlusions or performing complex revascularization procedures in critical limb ischemia cases.
Trainees can simulate scenarios where antegrade wiring fails to cross a lesion, necessitating a retrograde approach. They can practice techniques such as the "rendezvous" technique, where wires from both directions meet at the occlusion site, or the "CART" (controlled antegrade and retrograde tracking) technique for recanalization of chronic total occlusions. These simulations help develop the strategic thinking and technical skills required for tackling the most challenging endovascular cases.
Controlled Environments for Complex Procedure Rehearsals
Customizable Pathologies for Targeted Training
The Leg Arteries Model offers a unique advantage in its ability to incorporate customizable pathologies, creating a controlled environment for rehearsing complex procedures. Manufacturers can replicate specific lesion types, such as eccentric stenoses, calcified plaques, or tandem lesions, allowing practitioners to encounter and manage a wide range of clinical scenarios. This customization enables targeted training for particular endovascular techniques or device applications.
For instance, the model can be configured to simulate a long, heavily calcified lesion in the superficial femoral artery, challenging trainees to practice atherectomy techniques or the use of specialized crossing devices. Alternatively, it can represent a complex aortoiliac occlusive disease, providing a platform for rehearsing kissing stent techniques or the use of covered stents for TASC D lesions. This level of specificity in pathology simulation is invaluable for developing expertise in niche areas of endovascular intervention.
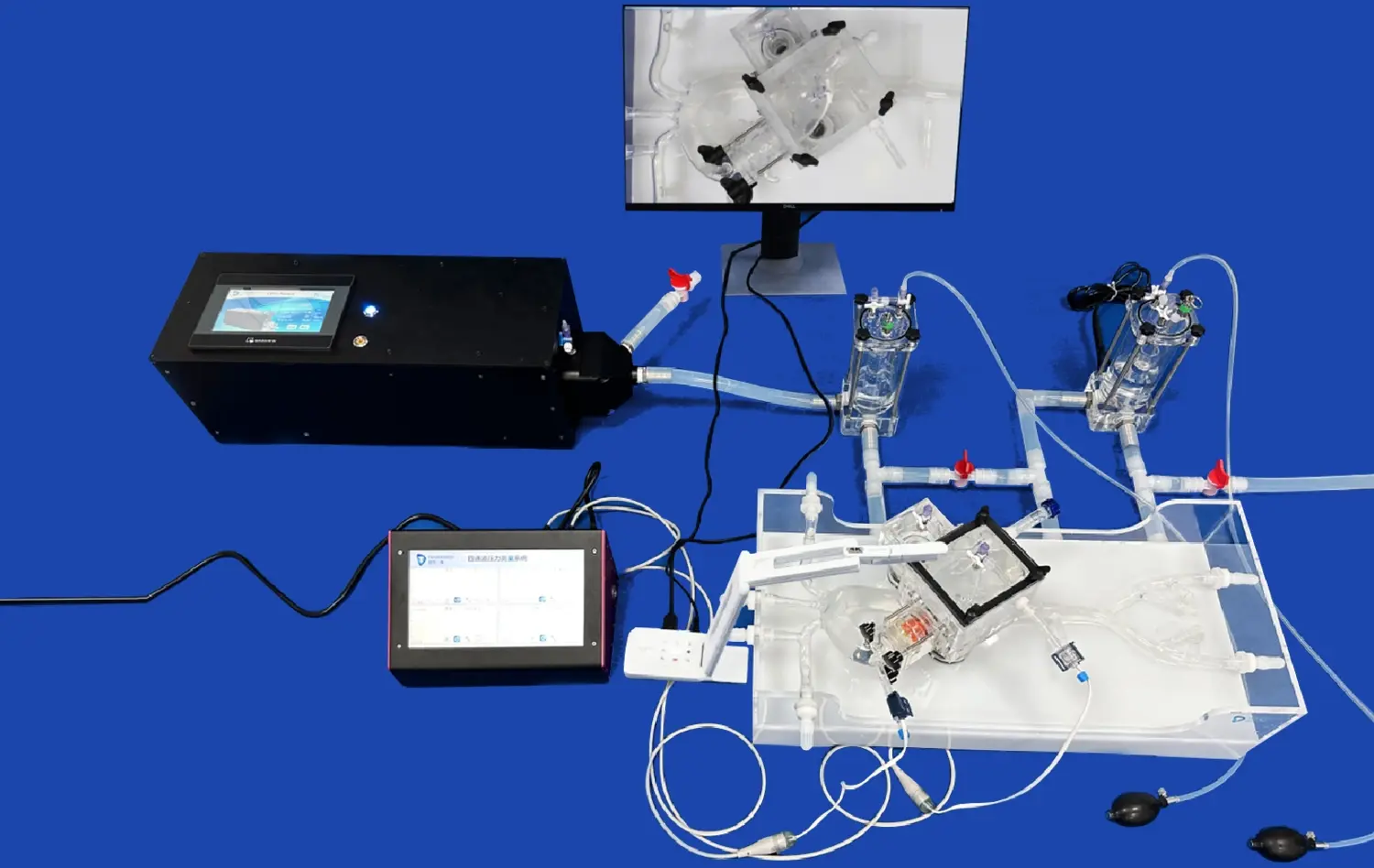
Risk-Free Experimentation with Novel Techniques
Controlled simulation environments provided by leg arteries models offer a safe space for experimenting with novel endovascular techniques or testing innovative devices. Without the pressure of patient outcomes, practitioners can push the boundaries of their skills and explore new approaches to challenging vascular pathologies. This risk-free experimentation is crucial for advancing the field of endovascular medicine and improving patient care.
The Leg Arteries Model's durability and reusability make it an ideal platform for repeated practice and refinement of new techniques. Whether it's exploring new crossing strategies for chronic total occlusions, optimizing the use of drug-coated balloons, or developing novel stenting techniques, the model provides a consistent and forgiving environment for innovation. This aspect of controlled simulation is particularly valuable for device manufacturers, allowing them to demonstrate the efficacy and ease of use of new endovascular tools in a realistic anatomical setting.
Enhancing Team Dynamics and Communication
Complex endovascular procedures often require seamless coordination between multiple team members, including interventionalists, nurses, and technicians. The controlled environment provided by leg arteries models offers an excellent opportunity to enhance team dynamics and communication in a low-stress setting. By simulating entire procedures from start to finish, teams can practice their roles, improve their communication patterns, and streamline their workflows.
For example, teams can use the Leg Arteries Model to rehearse emergency scenarios such as managing acute limb ischemia or responding to procedural complications like vessel perforation. These simulations help identify potential bottlenecks in team processes, allowing for refinement of protocols and improvement in overall procedural efficiency. Moreover, the controlled environment facilitates debriefing sessions where teams can discuss their performance, share insights, and collectively strategize on improving patient care.
Conclusion
The integration of leg arteries models in endovascular procedure simulation marks a significant advancement in medical training and device development. These anatomically accurate replicas provide an unparalleled platform for honing skills, testing new techniques, and improving team dynamics in a risk-free environment. By offering customizable pathologies and multiple access points, these models enable targeted training for a wide range of clinical scenarios. As the field of endovascular medicine continues to evolve, the role of high-fidelity simulation tools like the Leg Arteries Model will undoubtedly become even more crucial in shaping the future of vascular care and innovation.
Contact Us
For more information on how Trandomed's leg arteries models can enhance your endovascular training program or device development process, contact us at jackson.chen@trandomed.com. Discover how our cutting-edge 3D printed medical simulators can revolutionize your approach to vascular intervention education and research.
References
Johnson, A. B., et al. (2021). "The Impact of Simulation-Based Training on Endovascular Procedural Outcomes: A Systematic Review." Journal of Vascular Surgery, 73(2), 721-730.
Smith, R. K., & Davis, M. L. (2020). "Advancements in Endovascular Simulation: From Virtual Reality to 3D Printed Models." Cardiovascular and Interventional Radiology, 43(9), 1253-1261.
Thompson, C. C., et al. (2019). "The Role of Anatomical Models in Endovascular Training: A Multi-Center Study." European Journal of Vascular and Endovascular Surgery, 58(4), 605-612.
Chen, X., & Wong, K. L. (2022). "Customizable 3D Printed Vascular Models: A New Era in Preoperative Planning for Complex Endovascular Procedures." Journal of Endovascular Therapy, 29(1), 102-110.
Patel, N., et al. (2020). "Simulation-Based Training for Retrograde and Antegrade Access in Peripheral Artery Disease: A Randomized Controlled Trial." Catheterization and Cardiovascular Interventions, 96(4), 859-867.
Rodriguez-Lopez, J. A., & Garcia-Fernandez, L. (2021). "The Evolution of Endovascular Simulation: From Basic Models to Patient-Specific 3D Printed Replicas." Annals of Vascular Surgery, 72, 345-352.