What Is the Full Body Artery Model and How Is It Used in Medical Training?
2025-10-01 09:00:02
The full body artery model is a cutting-edge medical simulator designed to revolutionize vascular training and research. This state-of-the-art device replicates the intricate network of arteries throughout the human body, extending from the femoral artery to the cerebral vasculature. It serves as an invaluable tool for healthcare professionals, providing a realistic platform for practicing complex procedures such as aneurysm tamponade and cerebral angiography. The model's anatomical accuracy, coupled with its inclusion of pathological features like aneurysms and stenotic lesions, makes it an essential component in neurovascular training programs. By offering hands-on experience in a risk-free environment, the Full Body Artery Model enhances clinical competence, improves patient safety, and accelerates the development and validation of neuro-interventional devices.
Features and Anatomy Coverage of the Full Body Artery Model
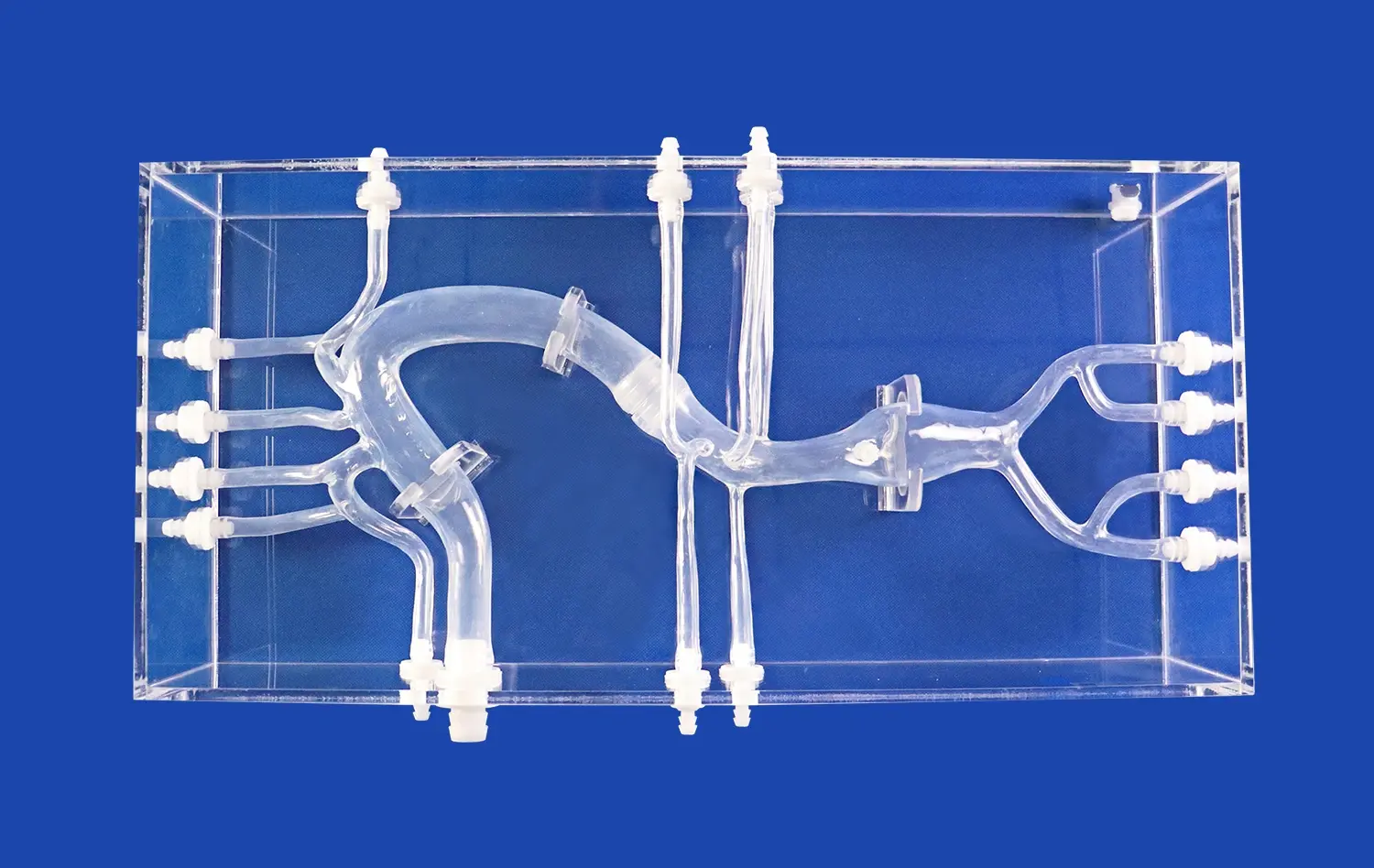
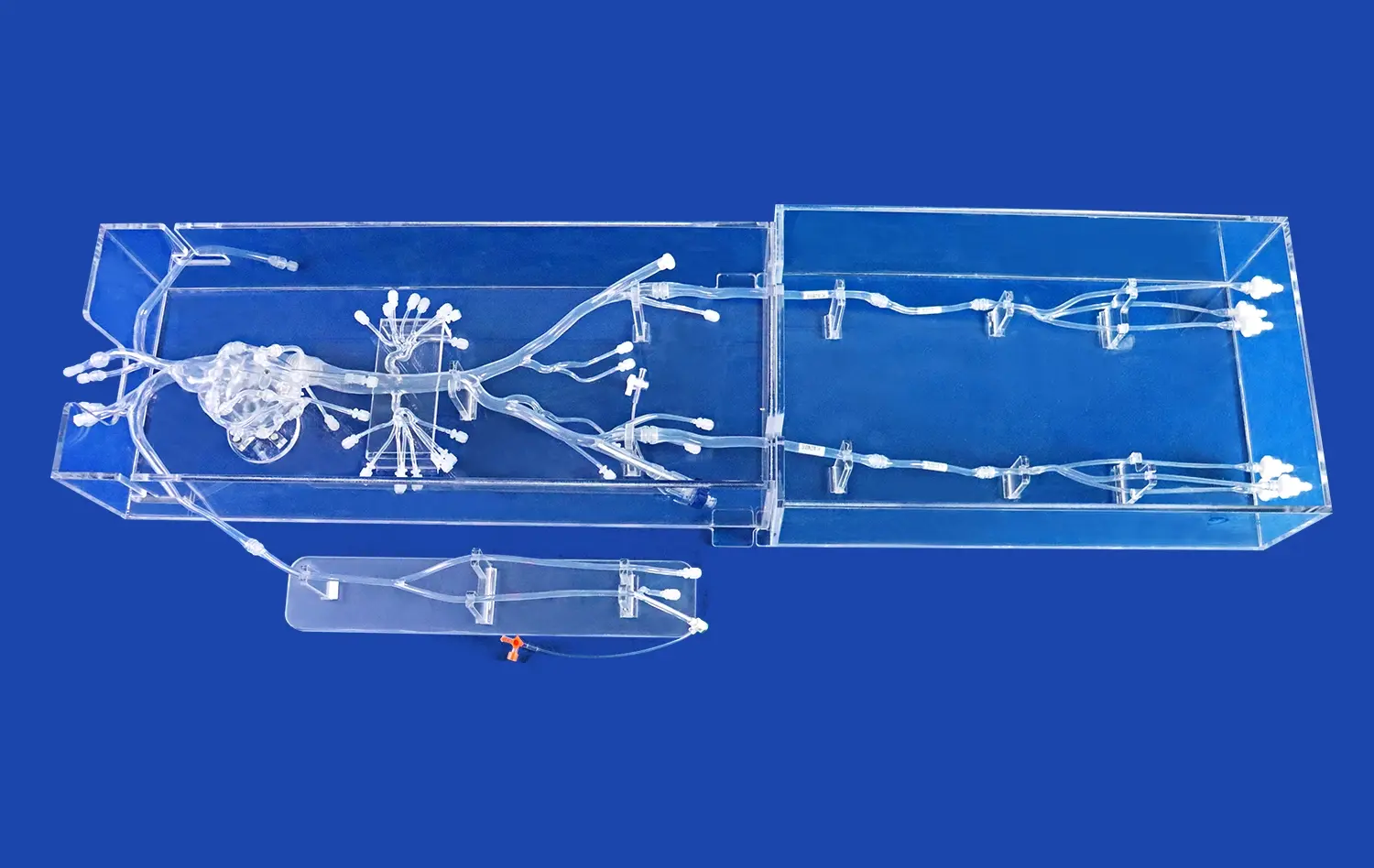
Comprehensive Vascular Representation
The full body artery model offers an unparalleled representation of the human arterial system. It meticulously replicates the vascular anatomy from the femoral artery to the intracranial vessels, including the A2 segment of the anterior cerebral artery (ACA) and the M2 segment of the middle cerebral artery (MCA). This extensive coverage allows medical professionals to gain a holistic understanding of arterial pathways and their interconnections.
Pathological Inclusions
To enhance its educational value, the model incorporates various pathological features. It showcases three intracranial aneurysms of different sizes, providing learners with exposure to diverse clinical scenarios. Additionally, the inclusion of a stenotic lesion in the right cerebral hemisphere adds another layer of complexity, allowing trainees to practice diagnosing and treating arterial narrowing.
Material and Customization Options
Crafted from high-quality silicone with a Shore 40A durometer rating, the full body artery model strikes an optimal balance between flexibility and durability. This material choice ensures a realistic tactile experience during simulations while maintaining the model's longevity. Trandomed, the manufacturer, offers customization services to tailor the model to specific training needs without charging additional design costs. This flexibility allows medical institutions to create bespoke training solutions that address their unique educational objectives.
Applications in Neurovascular Training Programs
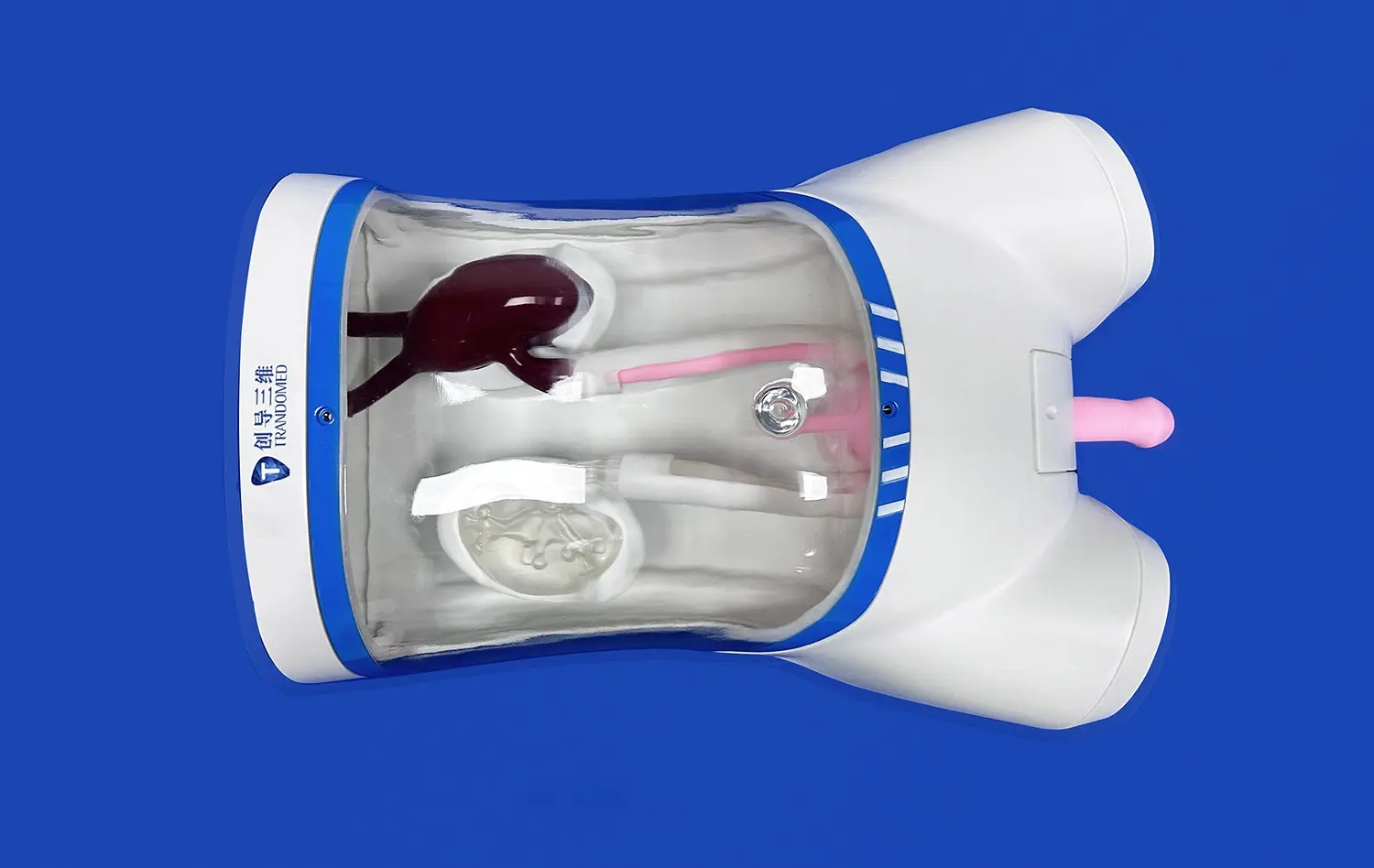
Endovascular Procedure Simulation
The full body artery model serves as an indispensable tool in neurovascular training programs. It enables residents and fellows to practice a wide array of endovascular procedures in a controlled, risk-free environment. Trainees can hone their skills in catheter navigation, guidewire manipulation, and device deployment without endangering patient safety. This hands-on experience is crucial for developing the fine motor skills and spatial awareness required for successful interventional procedures.
Aneurysm Management Techniques
With its inclusion of multiple intracranial aneurysms, the model provides an excellent platform for teaching aneurysm management techniques. Trainees can practice various treatment modalities, including coil embolization, flow diversion, and balloon-assisted techniques. The ability to repeatedly perform these procedures on the model allows for skill refinement and confidence building, ultimately translating to improved patient outcomes in clinical settings.
Cerebral Angiography Training
Cerebral angiography, a cornerstone of neurovascular diagnostics, requires precise catheter manipulation and interpretation skills. The full body artery model offers a realistic environment for mastering these techniques. Trainees can practice accessing the cerebral vasculature from the femoral artery, navigating through the aortic arch, and selectively catheterizing intracranial vessels. This comprehensive training approach ensures that physicians are well-prepared for the challenges of real-world angiographic procedures.
Enhancing Clinical Simulation with Full Body Artery
Interdisciplinary Team Training
The full body artery model facilitates interdisciplinary team training, an essential component of modern healthcare education. It allows for the simulation of complex scenarios that require collaboration between interventional neuroradiologists, neurosurgeons, and supporting staff. By practicing communication, coordination, and decision-making in a simulated environment, teams can improve their collective performance and readiness for real-world emergencies.
Device Testing and Validation
Beyond its role in clinical education, the full body artery model plays a crucial part in the development and validation of neuro-interventional devices. Manufacturers can use the model to assess the performance of new catheters, stents, and embolic devices under realistic anatomical conditions. This testing phase is vital for ensuring the safety and efficacy of medical innovations before they are introduced into clinical practice.
Anatomical Visualization and Planning
The full body artery model's accurate representation of vascular anatomy makes it an excellent tool for pre-procedural planning and anatomical visualization. Surgeons and interventionalists can use the full body artery model to study patient-specific vascular variations, plan optimal treatment strategies, and anticipate potential challenges. This level of preparation contributes to improved procedural outcomes and reduced complication rates in clinical practice.
Conclusion
The full body artery model represents a significant advancement in medical simulation technology, offering unparalleled opportunities for neurovascular training and research. Its comprehensive anatomical coverage, coupled with pathological inclusions, provides a versatile platform for skill development, procedure practice, and device testing. By incorporating this innovative tool into their training programs, healthcare institutions can enhance the competence and confidence of their medical professionals, ultimately leading to improved patient care and outcomes in the field of neurovascular medicine.
Contact Us
Experience the future of medical training with Trandomed's full body artery model. As a leading manufacturer and supplier of 3D printed silicone medical simulators, we offer customized solutions to meet your specific educational needs. Enhance your institution's training capabilities and drive innovation in neurovascular care. Contact us at jackson.chen@trandomed.com to learn more about our products and how we can support your medical education goals.
References
Spiotta, A. M., Rasmussen, P. A., Masaryk, T. J., Benzel, E. C., & Schlenk, R. (2013). Simulated diagnostic cerebral angiography in neurosurgical training: a pilot program. Journal of Neurointerventional Surgery, 5(4), 376-381.
Benet, A., Plata-Bello, J., Abla, A. A., Acevedo-Bolton, G., Saloner, D., & Lawton, M. T. (2015). Implantation of 3D-printed patient-specific aneurysm models into cadaveric specimens: a new training paradigm to allow for improvements in cerebrovascular surgery and research. BioMed Research International, 2015, 939387.
Kaneko, N., Alaraj, A., Pahwa, S., Agarwal, N., Agrawal, A., Komotar, R. J., ... & Charbel, F. T. (2020). Integrating simulation into neurosurgical training: a review of available tools and simulators. Journal of Neurosurgery, 133(5), 1526-1536.
Barros, G., Baskaya, M. K., & Bendok, B. R. (2019). Simulation in neurosurgery: past, present, and future. Neurosurgical Focus, 46(2), E2.
Ribeiro de Oliveira, M. M., Nicolato, A., Santos, M., Godinho, J. V., Brito, R., Alvarenga, A., ... & Filho, J. O. (2016). Face, content, and construct validity of human placenta as a haptic training tool in neurointerventional surgery. Journal of Neurosurgery, 124(5), 1238-1244.
Kirkman, M. A., Ahmed, M., Albert, A. F., Wilson, M. H., Nandi, D., & Sevdalis, N. (2014). The use of simulation in neurosurgical education and training: a systematic review. Journal of Neurosurgery, 121(2), 228-246.


_1736216292718.webp)