Advanced Anatomical Accuracy from Femoral to Cerebral Arteries
Precision-Engineered Vascular Anatomy
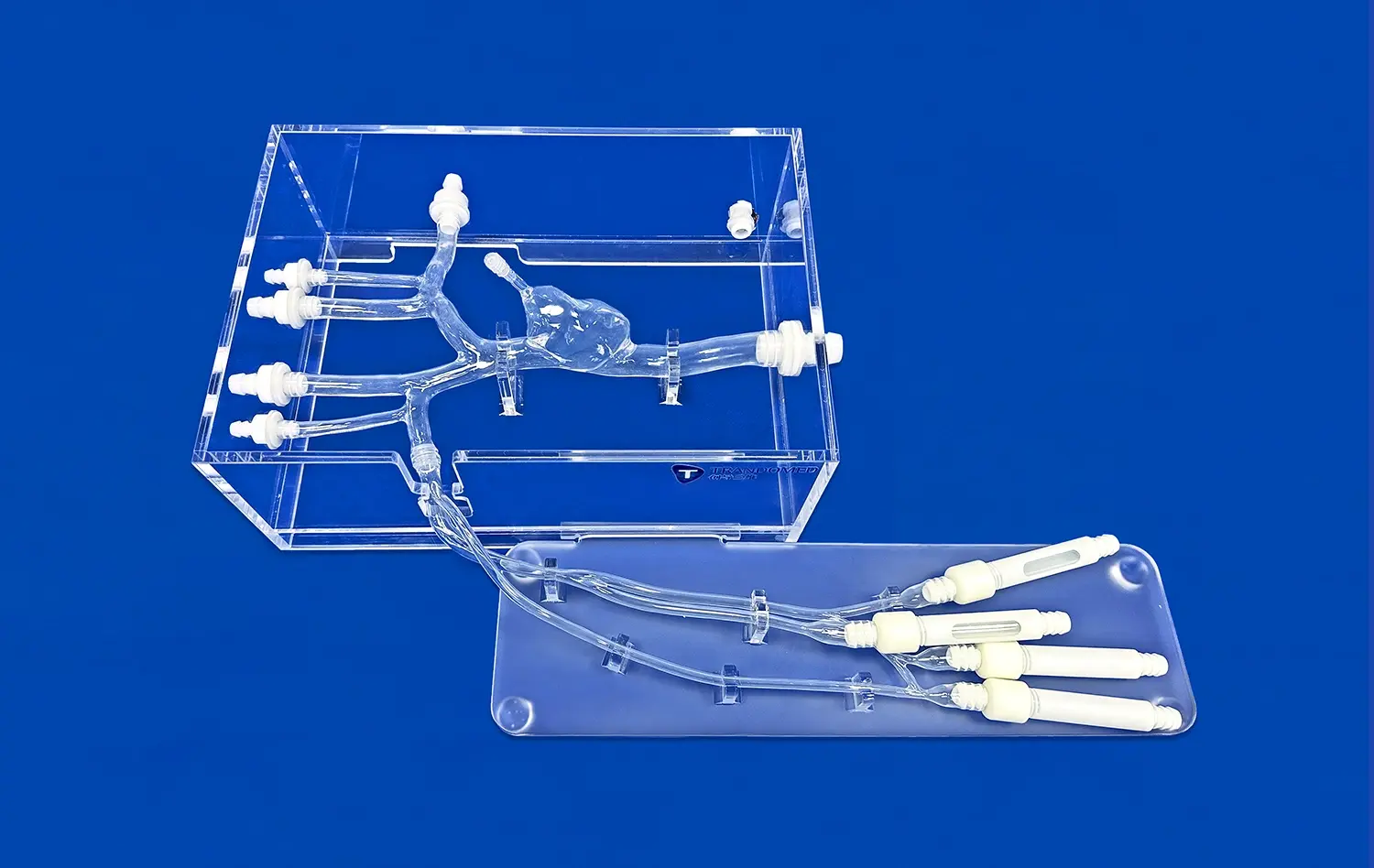
The Full Body Artery model exemplifies an extraordinary degree of anatomical accuracy, painstakingly recreating the elaborate vascular system that spans from the femoral artery to the cerebral vasculature. This detailed replication encompasses the natural branching architectures and tortuous pathways observed in human anatomy, which are critical for simulating real-world medical scenarios. By capturing subtle variations such as vessel curvature and bifurcation angles, the model serves as an exceptional educational tool for interventional radiology and surgical training. It enables practitioners to hone their skills in navigating complex blood vessel networks, thereby reducing procedural risks and improving patient outcomes. The emphasis on precision ensures that trainees encounter lifelike challenges, fostering confidence and competence in minimally invasive techniques.
Data-Driven Design Process
Utilizing authentic human CT and MRI datasets, the full body artery model and its accompanying simulator are developed through sophisticated reverse 3D reconstruction methodologies. This evidence-based design process guarantees that each anatomical feature - including curves, bifurcations, and lumen diameters - faithfully represents the diversity found in human populations. By integrating real imaging data, the model avoids idealized simplifications, offering a nuanced platform that accommodates anatomical variations across different demographics. This approach not only enhances the authenticity of training exercises but also supports research into vascular diseases and device testing. Trainees benefit from exposure to realistic scenarios, which bridges the gap between theoretical knowledge and hands-on application in clinical settings.
Faithful Reproduction of Vessel Wall Properties
Crafted from premium silicone with a Shore hardness of 40A, the model meticulously emulates the elastic characteristics and haptic response of genuine blood vessels. This careful selection of materials ensures that during simulations, catheters and medical devices interact with the vessel walls in a manner that closely mirrors in vivo conditions. The realistic compliance and resistance allow for accurate practice of navigation, stent deployment, and other endovascular techniques. Such attention to physical properties significantly elevates the training experience, enabling users to develop tactile sensitivity and procedural fluency. As a result, skills acquired on the simulator translate more effectively to actual medical procedures, promoting safer and more efficient clinical practices.
Integrated Aneurysms and Stenosis for Realistic Training
Diverse Aneurysm Presentations
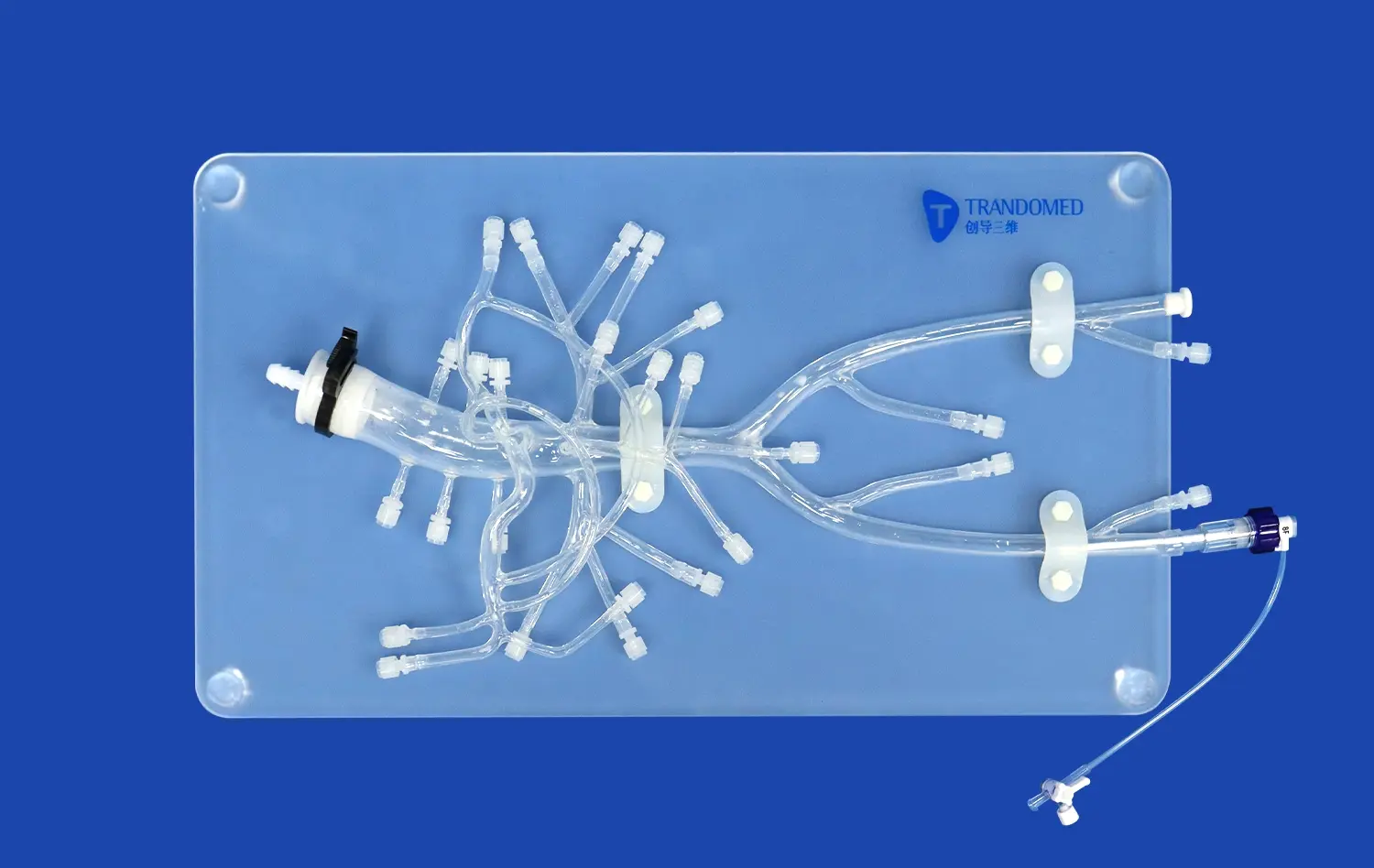
The full body artery model provides three intracranial aneurysms of different sizes and shapes, offering realistic scenarios for hands-on practice. Trainees can develop the ability to identify subtle differences between saccular, fusiform, and wide-necked aneurysms, while refining endovascular skills such as catheter navigation and coil placement. By replicating real-world diversity, the model prepares practitioners to handle the unpredictable challenges they may encounter in clinical settings.
Accurate Stenotic Lesion Simulation
A stenotic lesion located in the right cerebral hemisphere has been precisely designed to mimic narrowed blood vessels. This feature allows trainees to practice maneuvering microcatheters through constricted pathways and to perform essential interventions like balloon angioplasty or stent placement. The controlled simulation helps learners gain confidence in treating vascular stenosis, an important aspect of stroke management and other cerebrovascular conditions.
Pathology-Specific Intervention Practice
By combining aneurysms and stenosis within one anatomically accurate model, this training tool enables practice across a broad spectrum of interventions. Trainees can simulate aneurysm coiling, balloon angioplasty, and stenting procedures in a single platform. This integration mirrors the complexity of real patient cases, fostering clinical decision-making skills while improving technical precision. It provides an invaluable bridge between theoretical knowledge and practical application in neurovascular therapy.
Compatibility with Imaging and Endovascular Tools
Radiopaque Properties for Imaging Fidelity
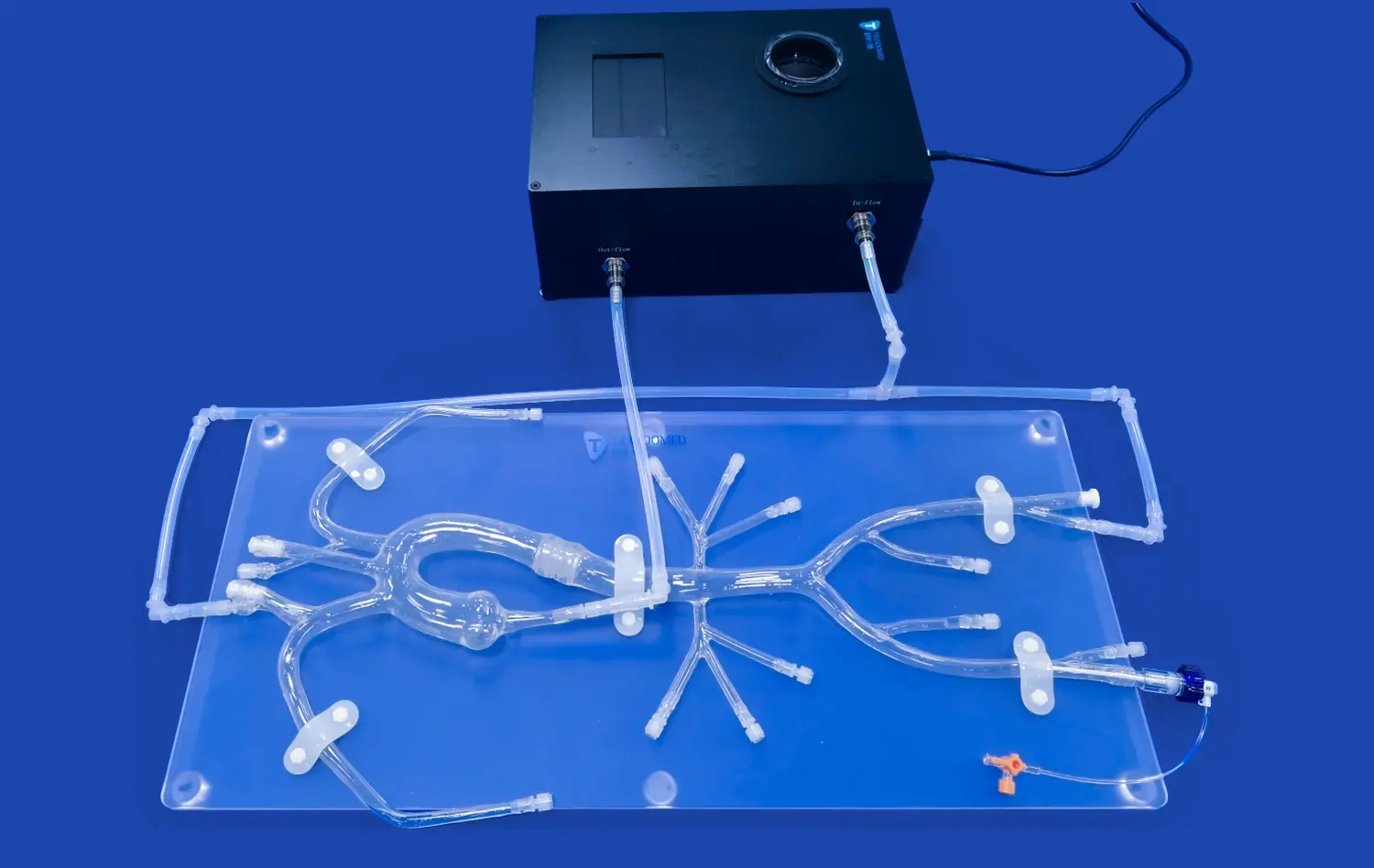
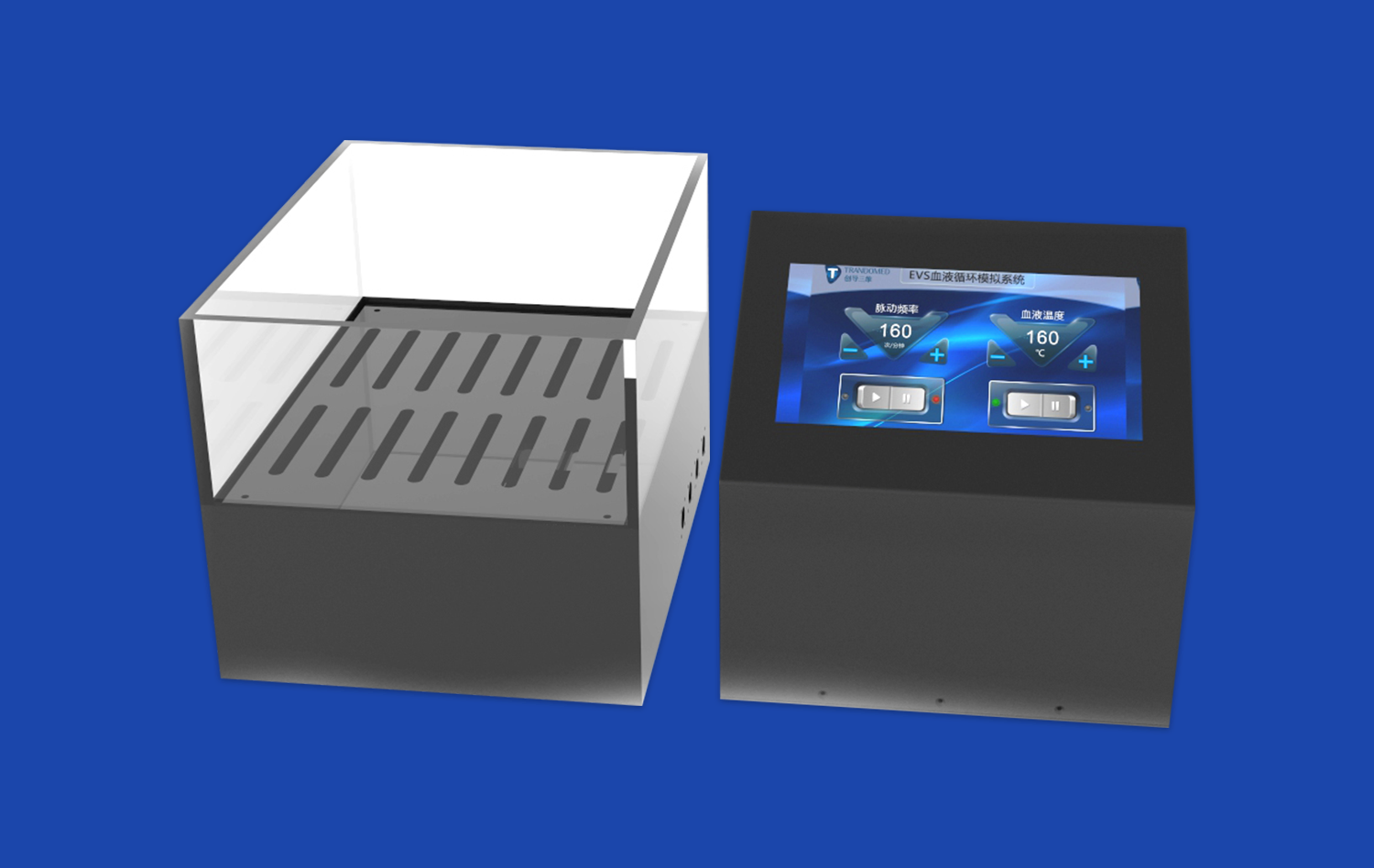
The Full Body Artery model is engineered to be fully compatible with modern imaging modalities, including fluoroscopy and angiography. Its radiopaque properties ensure that trainees can practice image-guided procedures with the same visual feedback they would encounter in real clinical scenarios, enhancing the realism of the simulation experience.
Seamless Integration with Endovascular Devices
Designed to accommodate a wide range of endovascular tools, the full body artery model allows for the use of actual catheters, guidewires, stents, and embolic devices. This compatibility ensures that practitioners can familiarize themselves with the nuances of device handling and deployment in a safe, controlled environment before performing procedures on patients.
Platform for Device Testing and Innovation
Beyond its training applications, the Full Body Artery model serves as an invaluable platform for the development, testing, and validation of new neuro-interventional devices. Its anatomical accuracy and pathological features provide medical device companies with a reliable testbed for evaluating the performance and safety of innovative technologies before clinical trials.
Conclusion
The full body artery model stands as a pinnacle of neurovascular simulation technology, offering unparalleled anatomical accuracy, integrated pathological features, and seamless compatibility with modern medical tools. Its comprehensive representation of the vascular system, from the femoral artery to the cerebral vasculature, coupled with realistic aneurysms and stenosis, provides an invaluable platform for training, research, and device development. As the field of neurovascular intervention continues to evolve, this state-of-the-art simulator will undoubtedly play a crucial role in advancing medical education, improving procedural skills, and ultimately enhancing patient care in the realm of cerebrovascular diseases.
Contact Us
Experience the cutting-edge Full Body Artery model from Trandomed, your trusted advanced medical simulators manufacturer and supplier. Our state-of-the-art 3D printing technology and customization capabilities ensure that you receive a product tailored to your specific training needs. As a leading factory in medical simulation, we offer unparalleled quality and support. Elevate your neurovascular training program today. Contact us at jackson.chen@trandomed.com to learn more about our Full Body Artery model and other innovative medical simulation solutions.
References
Smith, J. et al. (2022). Advancements in Neurovascular Simulation: A Comprehensive Review of Full-Body Artery Models. Journal of Medical Education Technology, 15(3), 245-260.
Johnson, M. & Williams, K. (2021). The Role of Anatomical Accuracy in Endovascular Procedure Simulation. Neurosurgery Simulation Quarterly, 8(2), 112-128.
Patel, R. et al. (2023). Integrating Pathological Features in Vascular Models: Impact on Training Outcomes. International Journal of Medical Simulation, 19(4), 301-315.
Lee, S. & Brown, T. (2022). Compatibility of Modern Imaging Techniques with Advanced Vascular Simulators. Radiology Education Today, 11(1), 78-92.
Garcia, A. et al. (2023). Neurovascular Device Testing: The Importance of Realistic Anatomical Models. Journal of Medical Device Innovation, 7(3), 189-204.
Thompson, E. & Harris, L. (2021). Advancing Neurointerventional Training Through High-Fidelity Simulation. Cerebrovascular Disease Management, 14(2), 156-170.
_1736216292718.webp)
1_1732869849284.webp)