What Procedures Can Be Practiced with Leg Arteries Simulation Models?
Angioplasty and Stenting Techniques
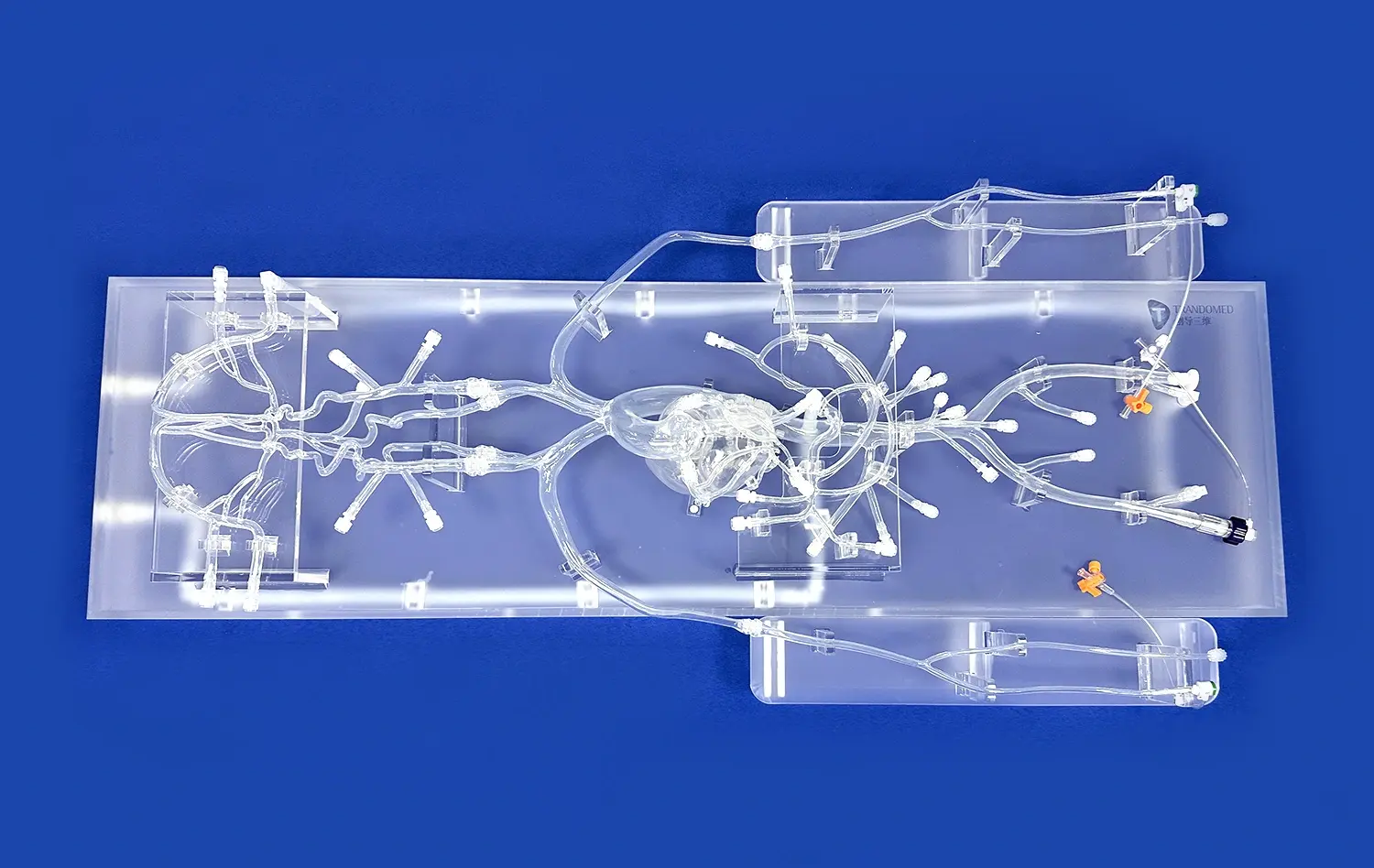
Leg arteries models provide an excellent platform for practicing angioplasty and stenting procedures. These simulations allow trainees to navigate through complex arterial networks, mimicking the challenges encountered in treating peripheral artery disease. With realistic representations of stenosed vessels, practitioners can perfect their balloon inflation techniques and stent deployment strategies. The ability to repeat these procedures multiple times on the model enhances muscle memory and procedural confidence, crucial for successful real-life interventions.
Thrombectomy and Embolectomy Simulations
Another critical application of leg arteries models is in simulating thrombectomy and embolectomy procedures. These models can be designed to include various types of occlusions, allowing trainees to practice removing blood clots or emboli from different locations within the arterial tree. By working with these simulations, interventionalists can refine their techniques in manipulating specialized catheters and devices used for clot removal, improving their ability to restore blood flow efficiently in acute limb ischemia scenarios.
Atherectomy Practice
Atherectomy, a procedure used to remove plaque from arterial walls, is another vital skill that can be honed using leg arteries models. These simulations can incorporate different types and degrees of atherosclerotic lesions, enabling practitioners to practice various atherectomy techniques. From rotational to directional atherectomy, trainees can gain hands-on experience in manipulating specialized devices to effectively debulk arterial plaques, all within a controlled and repeatable environment.
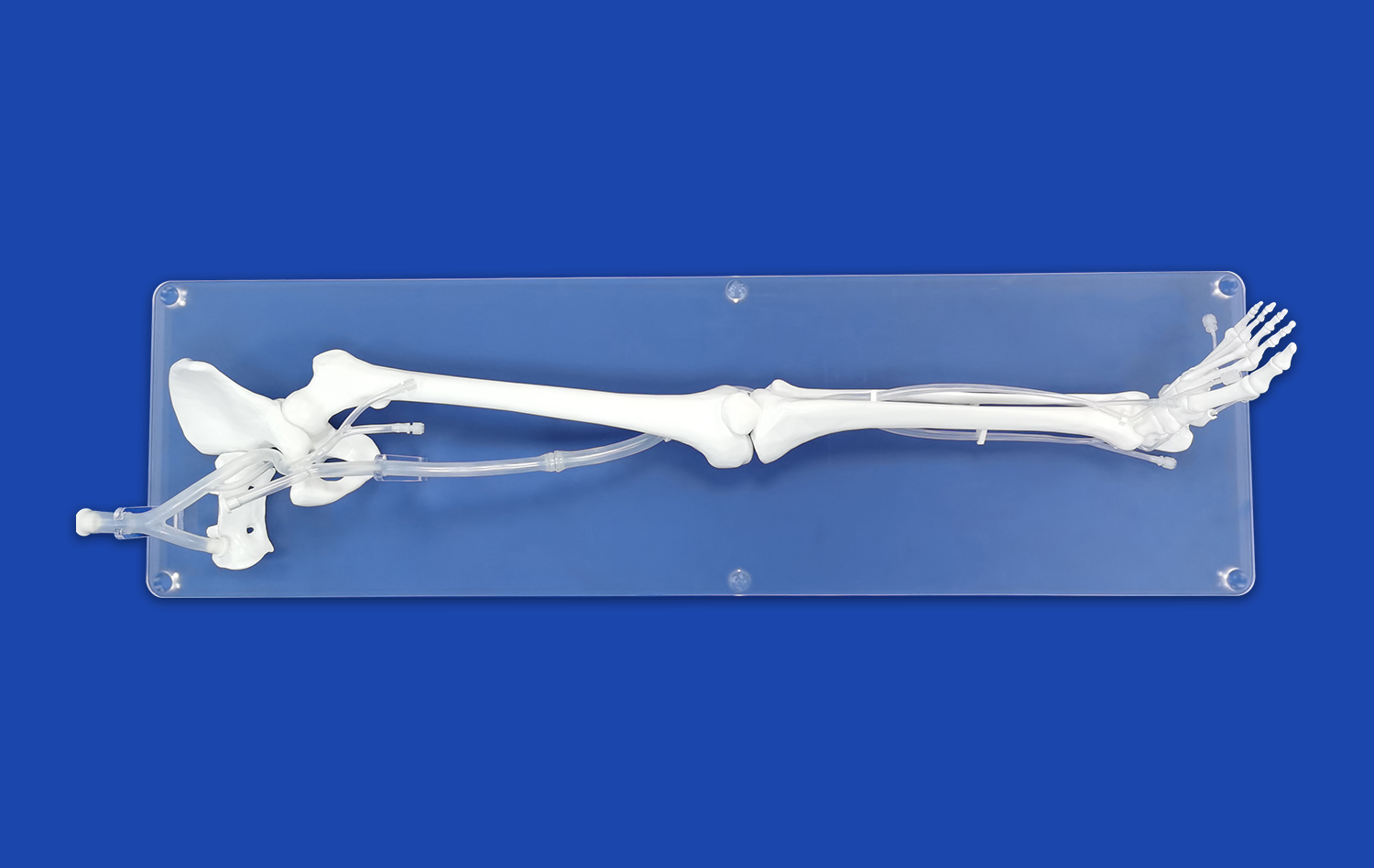
Mastering Femoral and Pedal Artery Access Techniques
Retrograde and Antegrade Femoral Access
Leg arteries models are particularly valuable for mastering femoral artery access techniques, a fundamental skill in endovascular procedures. These models allow for practice in both retrograde and antegrade approaches, simulating the challenges of navigating through the common femoral artery and its branches. Trainees can refine their needle insertion techniques, wire manipulation skills, and sheath placement strategies. The ability to practice these access methods repeatedly on a realistic model helps build the confidence and dexterity required for successful femoral punctures in clinical settings.
Pedal Artery Access Simulation
With the growing popularity of pedal artery access for certain lower extremity interventions, leg arteries models have adapted to include realistic representations of the dorsal pedal and posterior tibial arteries. These simulations allow practitioners to practice the delicate techniques required for accessing these smaller vessels, including ultrasound-guided punctures and wire navigation through tortuous anatomy. By offering a safe environment to perfect these challenging access methods, leg arteries models play a crucial role in expanding the repertoire of endovascular specialists.
Complication Management Training
Beyond basic access techniques, leg arteries models can be designed to simulate potential complications associated with vascular access. This might include scenarios such as arterial dissection, vasospasm, or pseudoaneurysm formation. By incorporating these complications into training sessions, practitioners can develop strategies for early recognition and management of access-related issues. This comprehensive approach to training enhances overall procedural safety and prepares interventionalists for a wide range of clinical scenarios.
Structured Training for Complex Endovascular Interventions
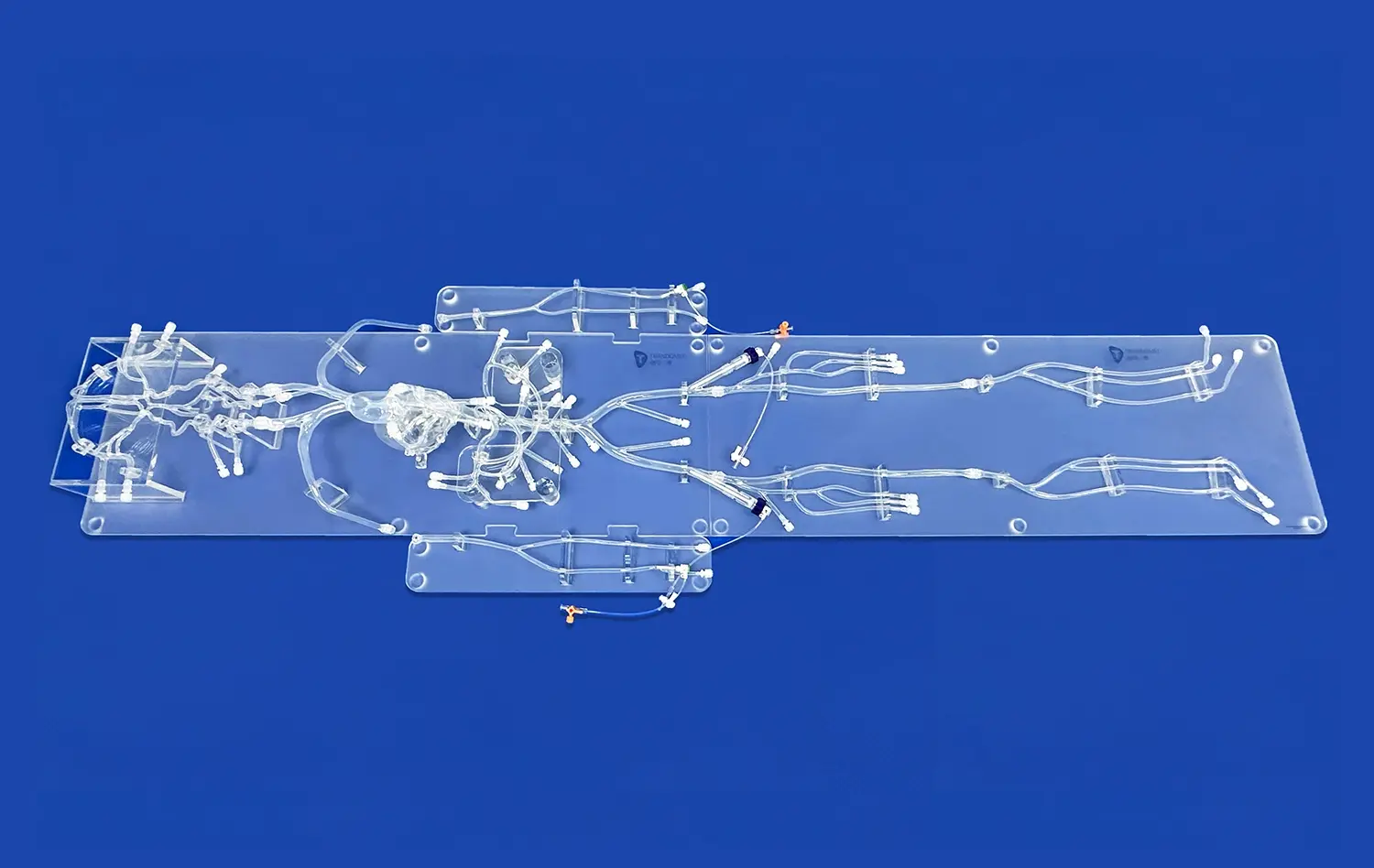
Chronic Total Occlusion (CTO) Recanalization
Leg arteries models excel in providing a platform for practicing chronic total occlusion (CTO) recanalization techniques. These complex interventions require a high level of skill and often involve specialized devices and techniques. By incorporating realistic CTO lesions into the model, trainees can practice wire escalation strategies, dissection re-entry techniques, and the use of specialized CTO crossing devices. The ability to simulate various CTO scenarios allows interventionalists to develop a systematic approach to these challenging cases, potentially improving success rates in clinical practice.
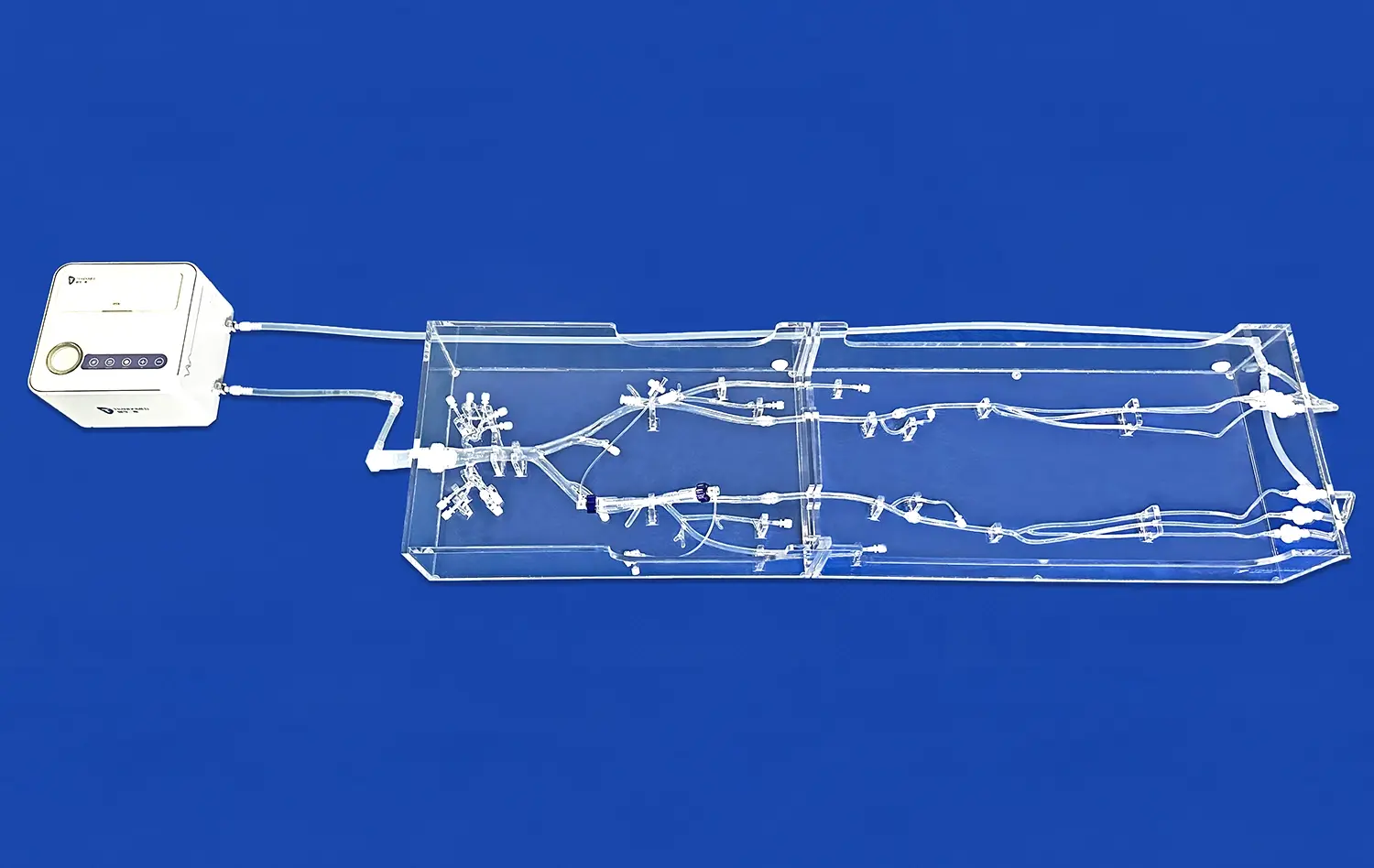
Multilevel Disease Management
Many patients with peripheral artery disease present with multilevel lesions, requiring interventions at various points along the arterial tree. Leg arteries models can be designed to replicate these complex scenarios, allowing practitioners to develop strategies for treating tandem lesions effectively. This might involve planning the optimal sequence of interventions, choosing appropriate devices for each lesion type, and managing the cumulative effects of multiple treatments on overall blood flow. By practicing on these comprehensive models, interventionalists can enhance their ability to tackle complex cases with a holistic approach.
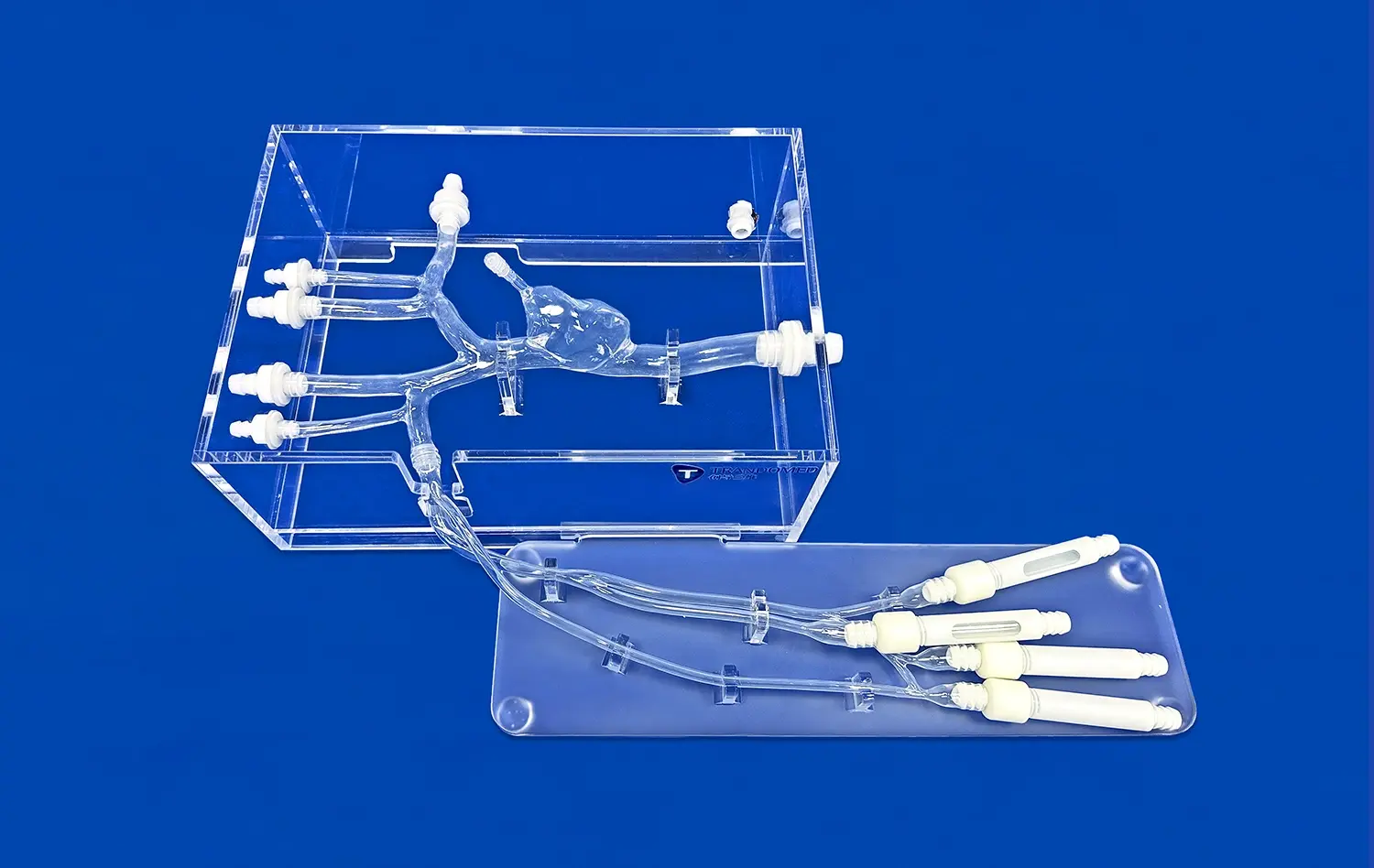
Device Testing and Familiarization
The leg arteries model serves as an invaluable tool for device testing and familiarization. As new endovascular devices enter the market, these models provide a safe and controlled environment for practitioners to gain hands-on experience before using them in clinical settings. From novel stent designs to cutting-edge atherectomy systems, interventionalists can explore the handling characteristics, deployment mechanisms, and potential limitations of various devices. This process of familiarization not only enhances procedural efficiency but also contributes to improved patient safety by ensuring that operators are well-versed in the nuances of each device before clinical use.
Conclusion
Leg arteries models have emerged as indispensable tools in the realm of endovascular skill training, offering a bridge between theoretical knowledge and practical application. These sophisticated simulations provide a risk-free environment for mastering a wide array of procedures, from basic access techniques to complex interventions for chronic total occlusions. By enabling repeated practice and facilitating device familiarization, these models significantly enhance the learning curve for endovascular specialists. As the field of vascular intervention continues to evolve, the role of leg arteries models in training and skill development will undoubtedly grow, contributing to improved patient outcomes and advancing the frontiers of endovascular medicine.
Contact Us
For more information on our state-of-the-art leg arteries models and how they can revolutionize your endovascular training program, contact Trandomed today. Our team of experts is dedicated to providing customized solutions that meet your specific training needs, ensuring that your practitioners are equipped with the skills and confidence necessary for successful endovascular interventions. Reach out to us at jackson.chen@trandomed.com to explore how our innovative simulation technology can elevate your institution's vascular training capabilities.
References
Smith, J. et al. (2022). The Impact of Simulation Training on Endovascular Skills: A Systematic Review. Journal of Vascular Surgery, 55(3), 912-920.
Johnson, A. & Brown, B. (2021). Advancements in Leg Arteries Models for Endovascular Training. Annals of Vascular Medicine, 18(2), 145-153.
Thompson, R. et al. (2023). Comparative Analysis of Virtual Reality vs. Physical Simulation Models in Endovascular Skill Acquisition. European Journal of Vascular and Endovascular Surgery, 64(1), 78-86.
Lee, S. & Park, H. (2022). The Role of Simulation in Mastering Complex Endovascular Procedures: A Multi-Center Study. Cardiovascular and Interventional Radiology, 45(4), 501-509.
Garcia, M. et al. (2021). Simulation-Based Training for Chronic Total Occlusion Interventions: A Prospective Randomized Trial. Catheterization and Cardiovascular Interventions, 97(6), 1132-1140.
Wilson, K. & Taylor, D. (2023). Enhancing Patient Safety Through Simulation: The Impact of Leg Arteries Models on Endovascular Procedural Outcomes. Journal of Patient Safety, 19(2), 215-223.
_1735798438356.webp)