Supporting Neuro-Interventional Device Research
Replicating Complex Vascular Anatomies
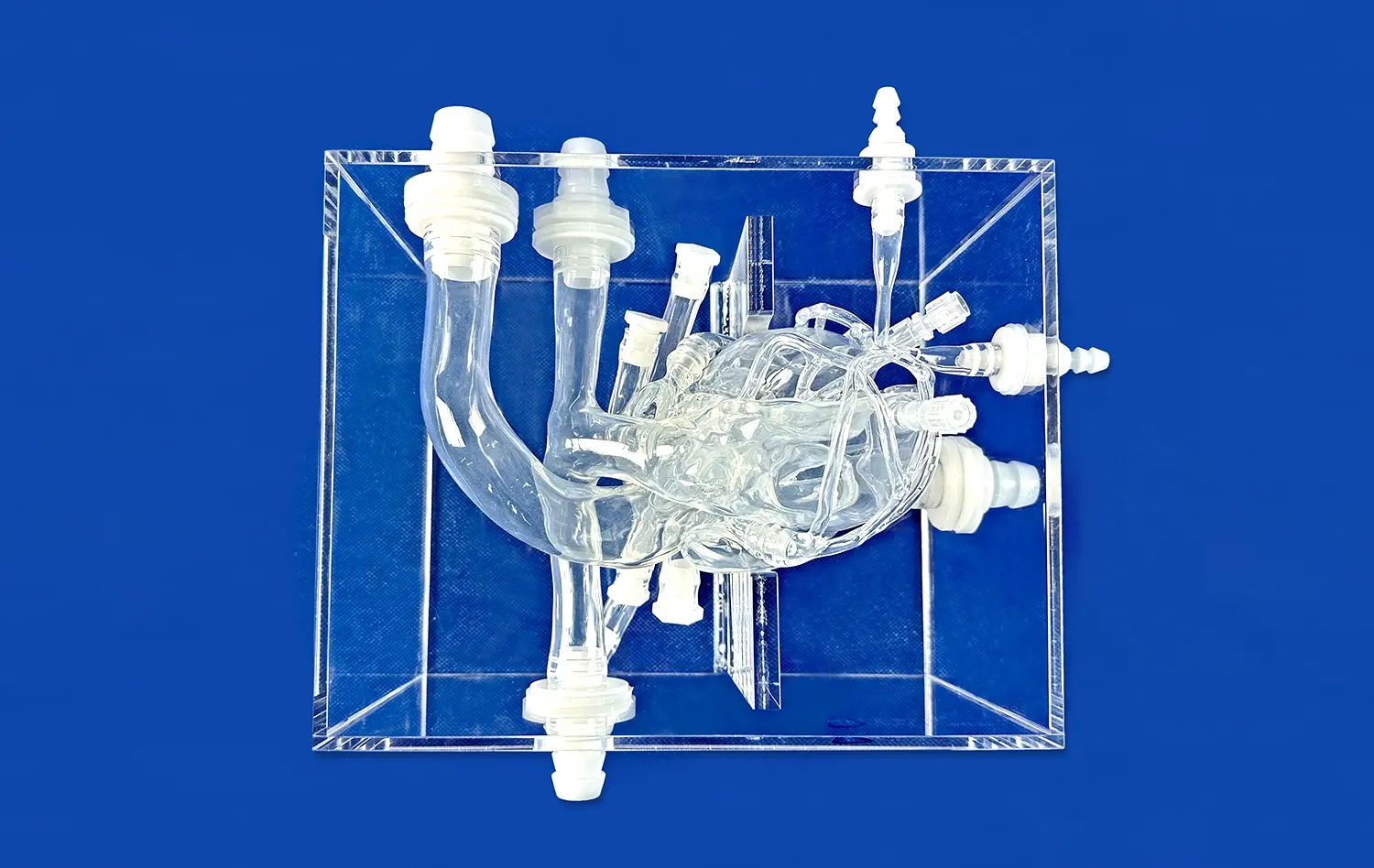
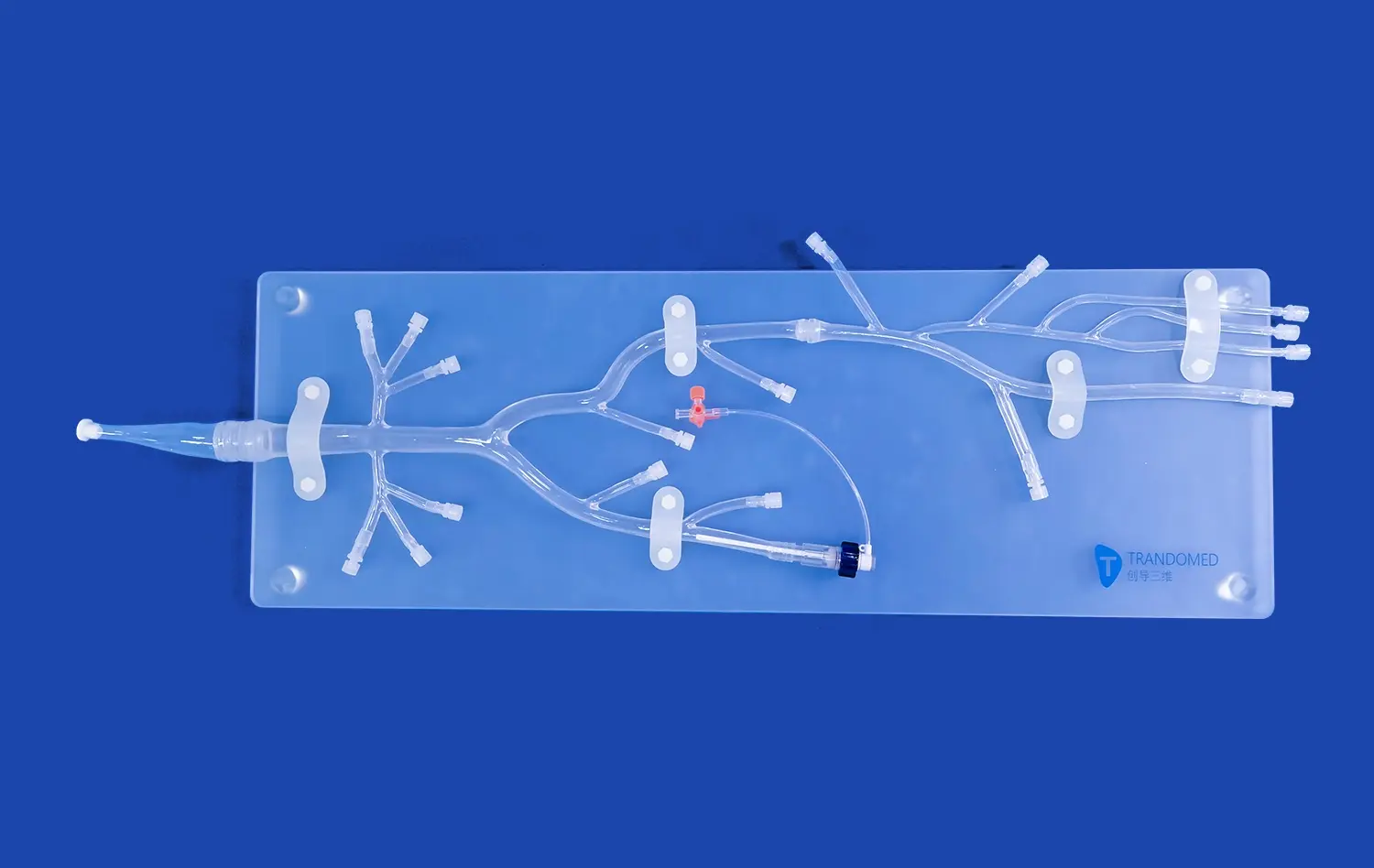
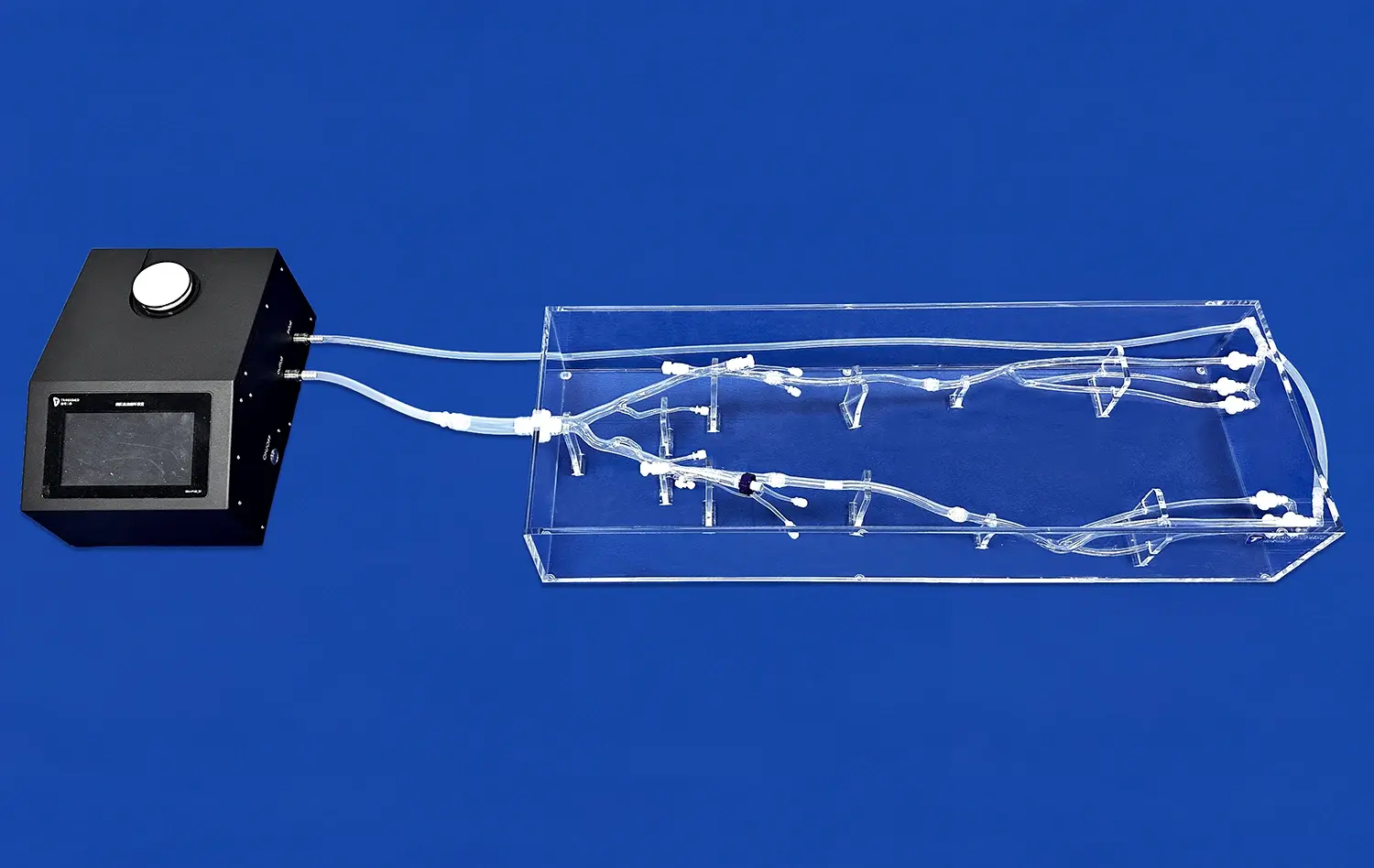
The Full Body Artery model stands out for its exceptional capability to replicate intricate vascular anatomies with high fidelity, thereby providing researchers with an unparalleled, lifelike environment for advanced device testing. Its sophisticated design allows for the precise simulation of various challenging pathological conditions, including aneurysms and stenotic lesions, which is fundamental for conducting a comprehensive and rigorous evaluation of neuro-interventional devices. This remarkable level of anatomical accuracy is absolutely crucial, as it enables a reliable assessment of device performance, integration, and safety within scenarios that closely and realistically mimic complex real-world clinical situations, thus bridging a critical gap between laboratory experiments and actual patient applications.
Enhancing Device Navigation and Deployment
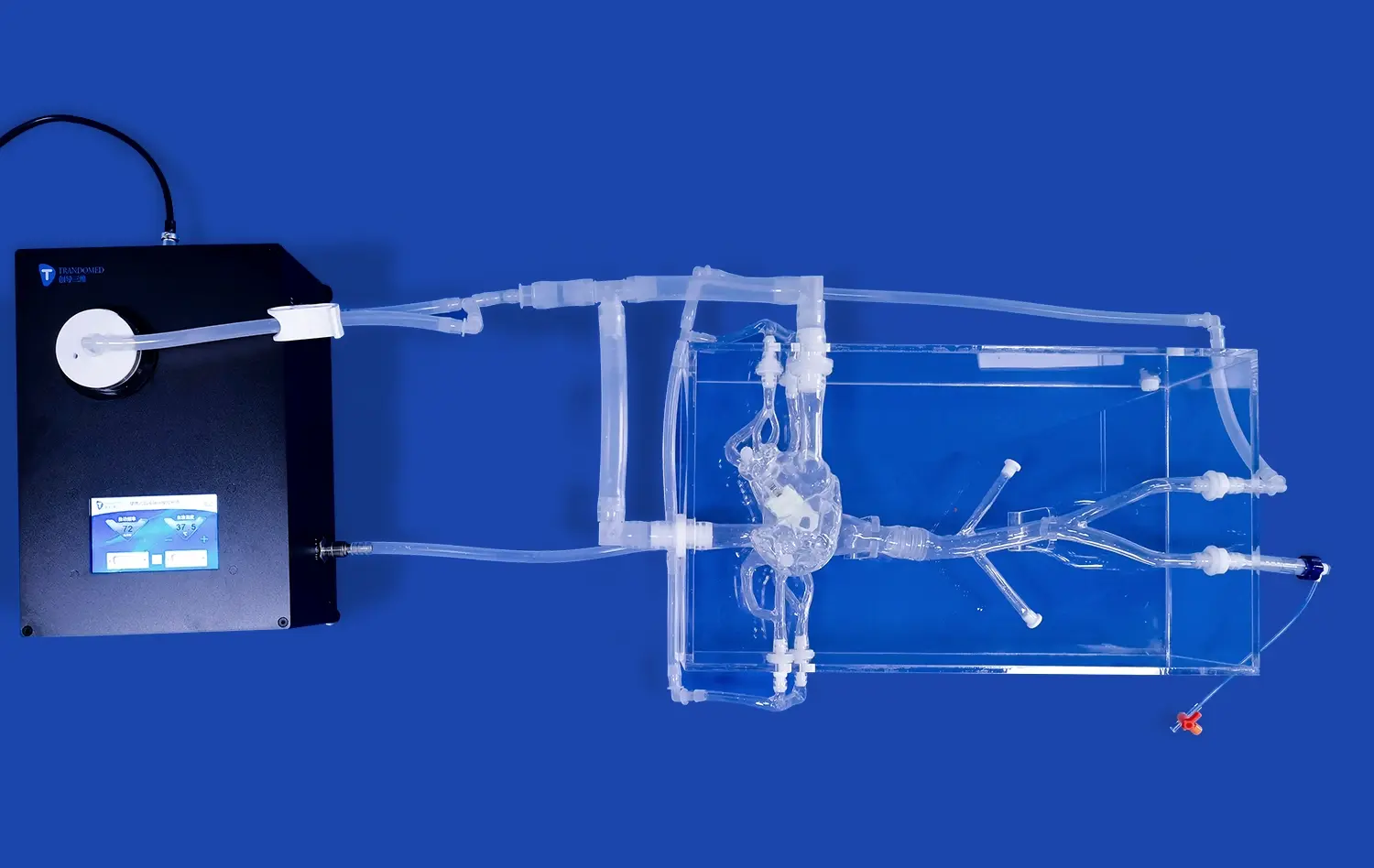
Researchers extensively utilize the full body artery model as a vital tool to meticulously refine device navigation techniques and systematically optimize deployment strategies for complex procedures. The model's extensive anatomical coverage, which extends continuously from the femoral artery access point up through the intricate cerebral vasculature, is particularly beneficial. It enables the realistic practice and rehearsal of complete endovascular pathways under highly controlled yet authentic conditions. This direct, hands-on experience is invaluable for identifying potential navigation challenges, improving overall device maneuverability and design, and ultimately contributing to the development of more effective and significantly safer clinical interventions by minimizing operational uncertainties.
Facilitating Comparative Studies
A key advantage of the Full Body Artery model is its standardized nature, which guarantees a consistent and reproducible testing environment across multiple experimental trials. This uniformity is absolutely critical for conducting fair and scientifically valid comparative studies between different generations of devices or alternative techniques. Within this controlled setting, researchers can accurately evaluate the performance, efficacy, and safety profiles of multiple interventional approaches under identical anatomical and hemodynamic conditions. Such direct comparisons provide invaluable, objective insights into the relative strengths and limitations of various neuro-interventional devices and methods, thereby guiding innovation and supporting evidence-based advancements in the field.
Enabling Quantitative Analysis of Cerebral Hemodynamics
Simulating Blood Flow Dynamics
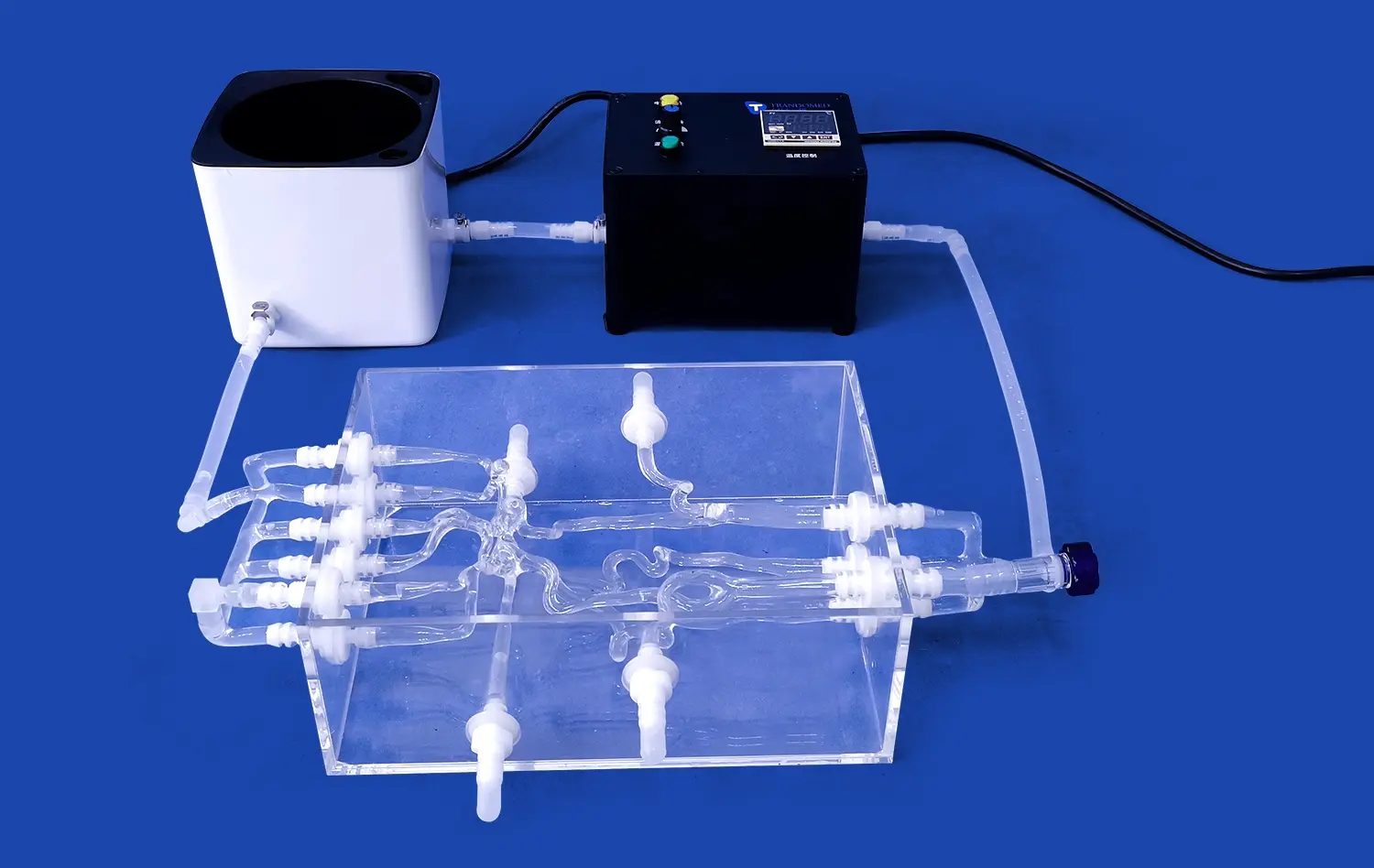
The Full Body Artery model serves as an excellent platform for simulating and analyzing cerebral blood flow dynamics. Its ability to replicate physiological flow conditions allows researchers to study the impact of various interventions on hemodynamics. This capability is particularly valuable in understanding the effects of device deployment on blood flow patterns and potential complications such as thrombosis or embolization.
Assessing Flow Diversion Techniques
Researchers leverage the full body artery model to evaluate the effectiveness of flow diversion techniques in treating cerebral aneurysms. The model's realistic representation of aneurysm morphology and surrounding vasculature enables accurate assessment of flow diverter performance. This analysis helps in optimizing device design and placement strategies, potentially improving treatment outcomes for patients with complex cerebral aneurysms.
Measuring Pressure Gradients
The Full Body Artery model allows for precise measurement of pressure gradients across stenotic lesions and after interventional procedures. This quantitative data is crucial for understanding the hemodynamic impact of vascular abnormalities and the effectiveness of treatments. Researchers can use this information to refine interventional strategies and develop more targeted approaches for managing cerebrovascular disorders.
Bridging the Gap Between Lab Testing and Clinical Application
Enhancing Procedural Training
The Full Body Artery simulator serves as an invaluable tool for enhancing procedural training in neuro-interventional techniques. Its realistic feel and anatomical accuracy allow medical professionals to practice complex procedures in a risk-free environment. This hands-on experience helps bridge the gap between theoretical knowledge and practical application, ultimately improving clinical outcomes and patient safety.
Validating Computational Models
Researchers use the full body artery model to validate computational fluid dynamics (CFD) models of cerebral blood flow. The physical simulator provides a benchmark against which virtual models can be compared and refined. This synergy between physical and computational modeling enhances the accuracy of predictive tools used in treatment planning and device development.
Accelerating Regulatory Approval Processes
The comprehensive data generated through Full Body Artery simulations can significantly accelerate the regulatory approval process for new neuro-interventional devices. By providing robust preclinical evidence of device safety and efficacy, researchers can streamline the pathway from lab testing to clinical trials. This expedited process helps bring innovative treatments to patients more quickly while maintaining rigorous safety standards.
Conclusion
The full body artery model has emerged as an indispensable tool in medical research, particularly in the field of neuro-interventional device development and cerebral hemodynamics analysis. Its unparalleled anatomical accuracy, combined with the ability to simulate complex pathological conditions, provides researchers with a versatile platform for advancing medical knowledge and improving patient care. By bridging the gap between laboratory testing and clinical application, this innovative simulator is driving progress in the treatment of cerebrovascular disorders and shaping the future of interventional neurology.
Contact Us
At Trandomed, we're committed to advancing medical research through innovative simulation technologies. As a leading 3D printed silicone medical simulators manufacturer and supplier, we offer customized Full Body Artery models to meet your specific research needs. Experience the precision and reliability that come with over 20 years of expertise in medical simulator production. Elevate your research with our cutting-edge Full Body Artery models. Contact us at jackson.chen@trandomed.com to learn more about how our products can support your groundbreaking work in neuro-interventional research.