What Makes the Model's Anatomical Precision Stand Out?
Unparalleled Realism in Vascular Structures
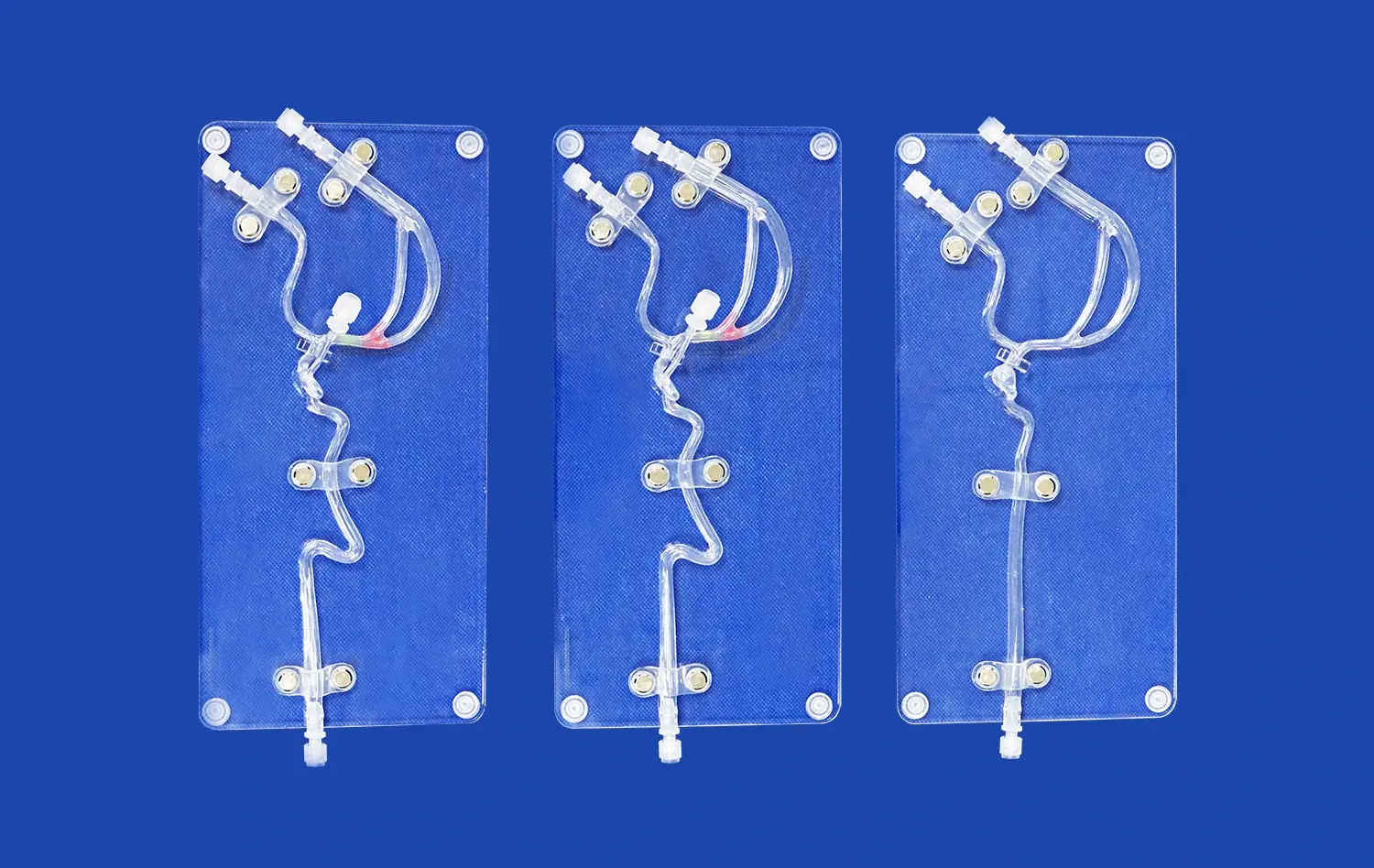
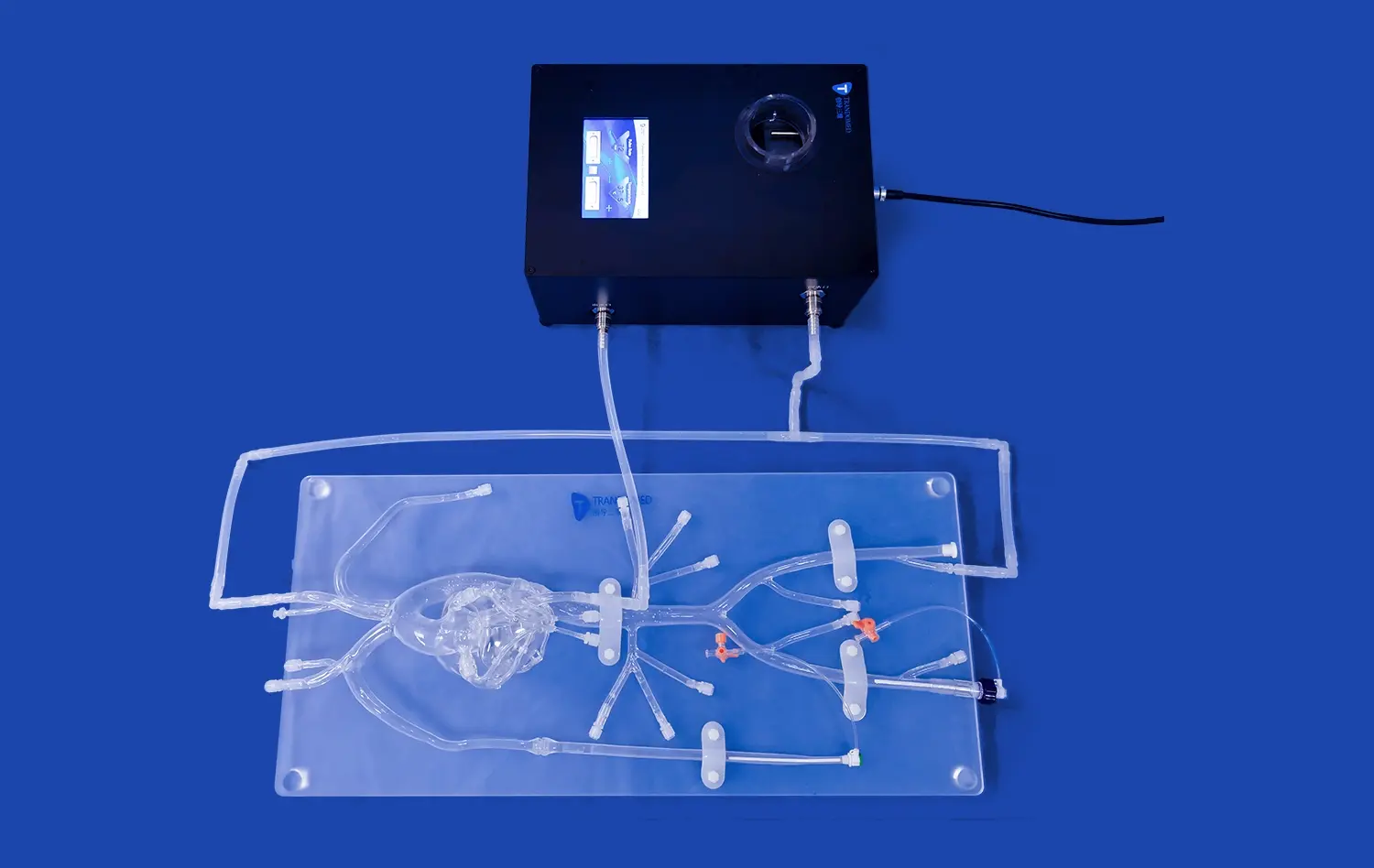
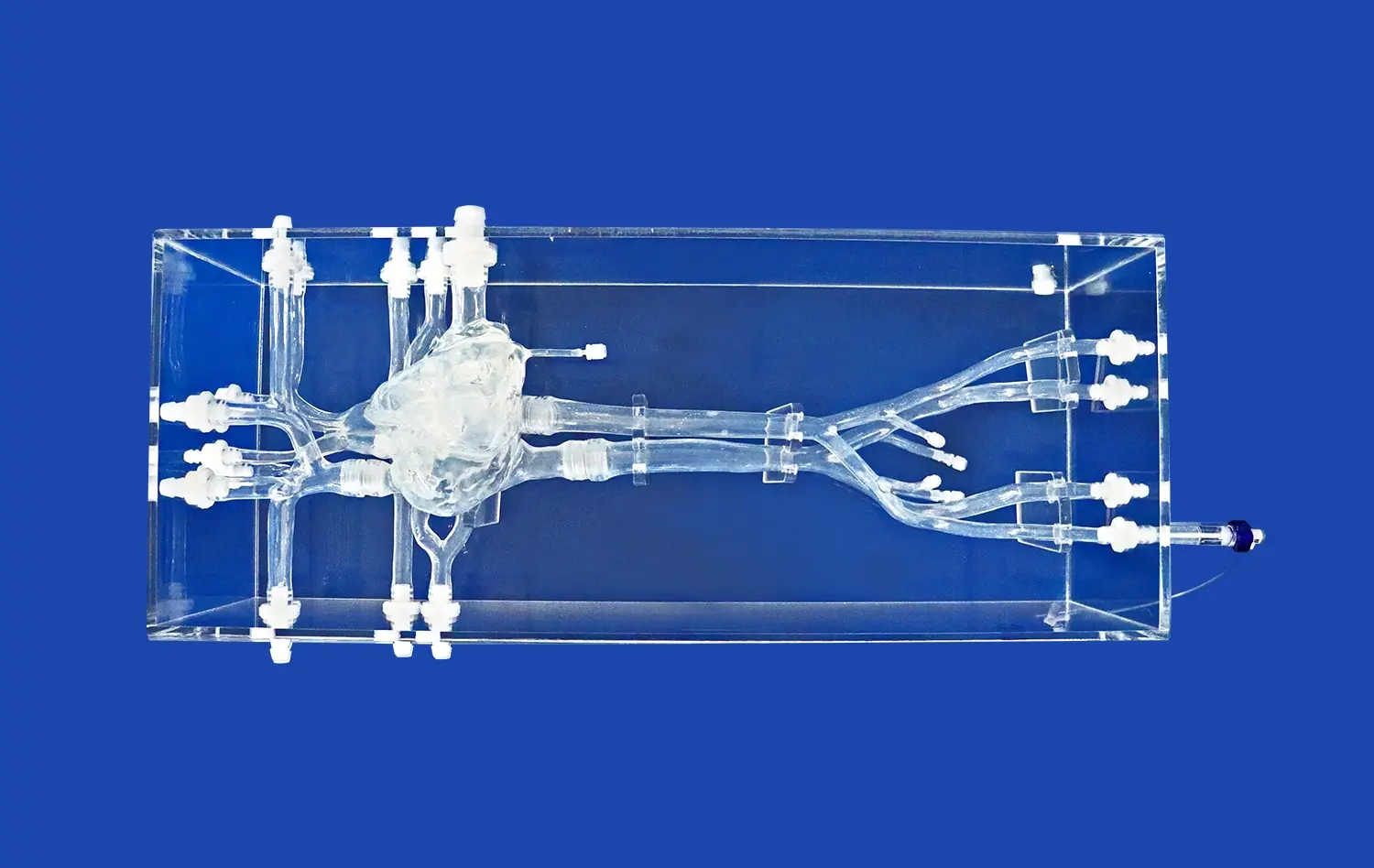
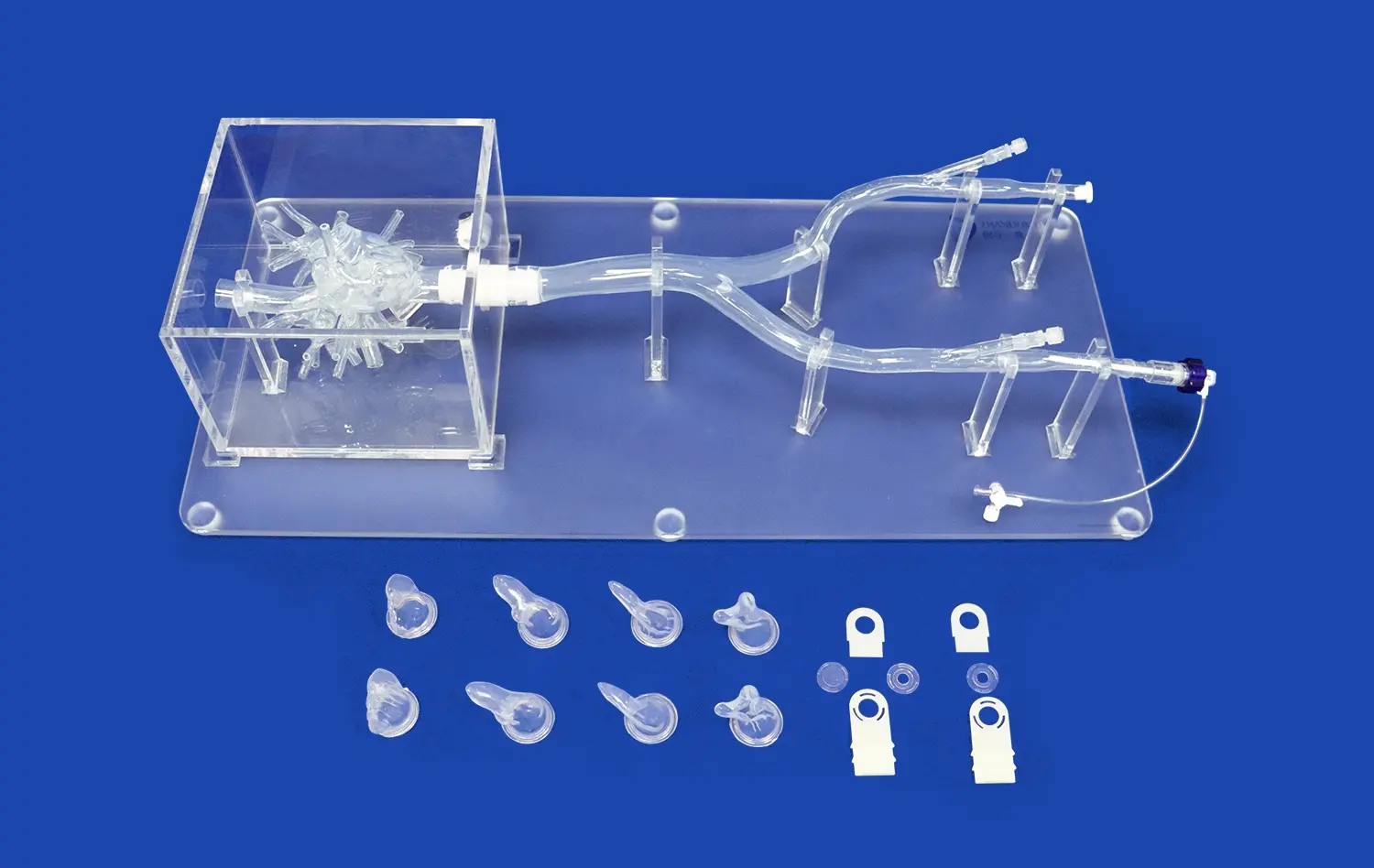
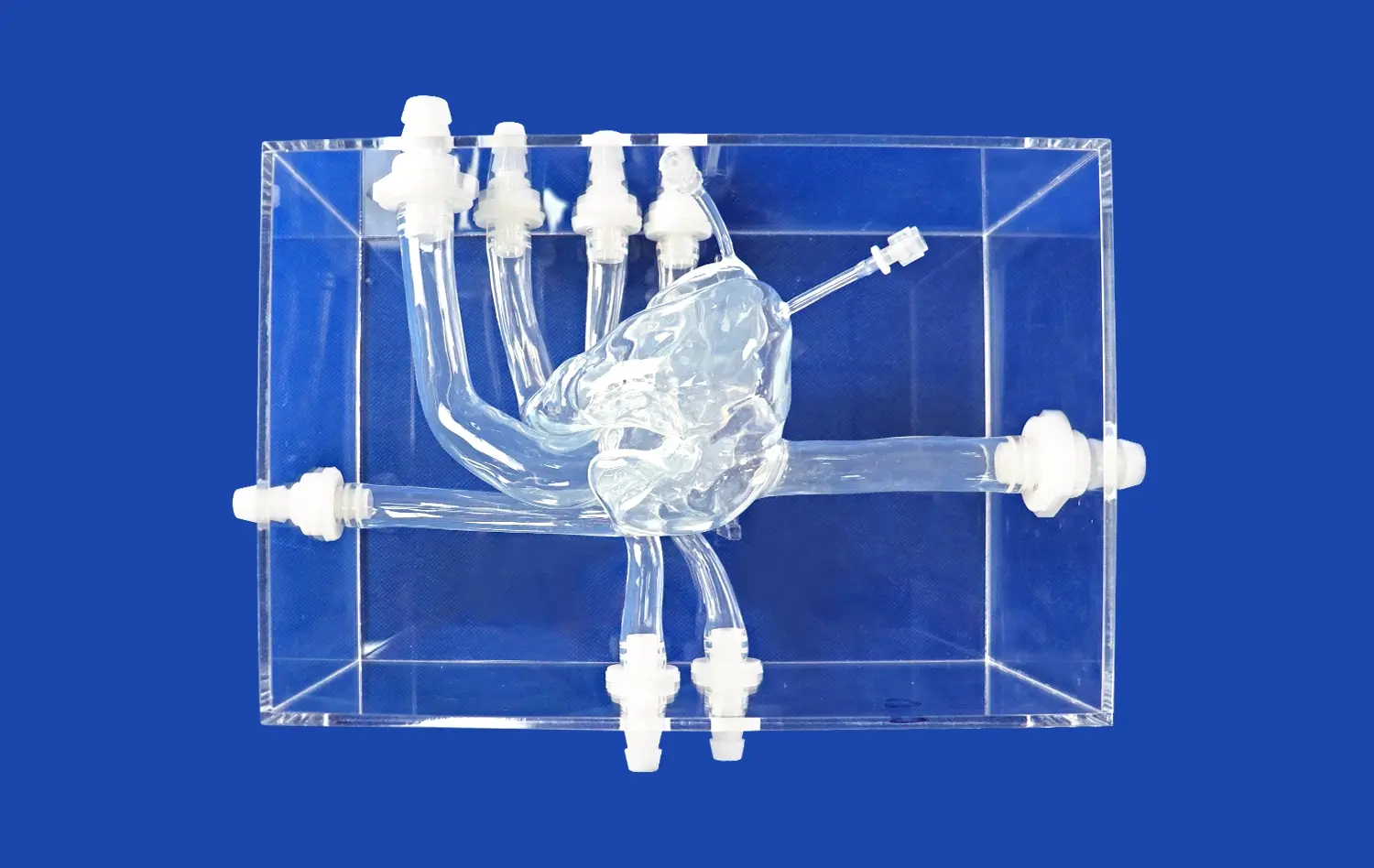
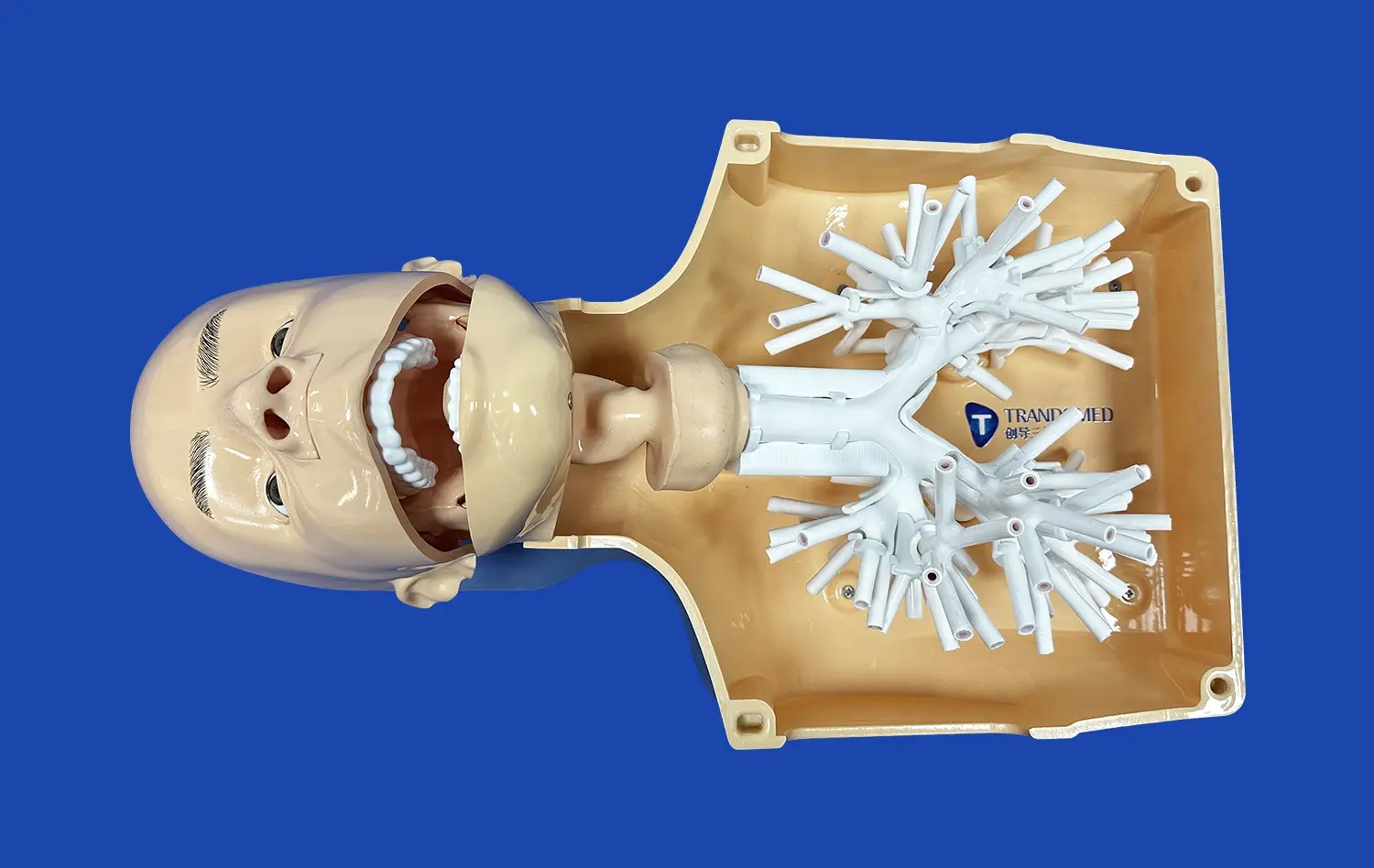
The lower extremity artery model sets a new standard in anatomical accuracy. By utilizing advanced 3D printing techniques and high-resolution CT data, these models capture even the most minute details of the vascular system. This level of precision is crucial for surgeons and researchers who need to understand the intricate network of arteries in the lower limbs. The models accurately replicate vessel diameters, branching patterns, and anatomical variations, providing a true-to-life representation that is invaluable for both training and research purposes.
Customization Based on Patient-Specific Data
One of the most significant advantages of these models is their ability to be customized based on individual patient data. This personalization allows surgeons to practice procedures on exact replicas of a patient's unique vascular anatomy before performing the actual surgery. For researchers, this customization capability opens up new avenues for studying rare anatomical variations and developing targeted treatment strategies. The ability to produce patient-specific models enhances the applicability of research findings and improves surgical outcomes by allowing for tailored approaches to complex cases.
Material Properties Mimicking Real Tissue
The choice of materials used in creating these models is crucial to their effectiveness. The silicone used in the lower extremity artery model, with its specific Shore hardness, closely mimics the properties of human blood vessels. This similarity in texture and elasticity allows for a realistic tactile experience during simulations. Surgeons can practice techniques such as catheter insertion, stent placement, and balloon angioplasty with a level of realism that closely approximates actual surgical conditions. For researchers, these material properties enable more accurate testing of new medical devices and treatment modalities, ensuring that their findings translate effectively to clinical applications.
Consistency and Reliability in Experimental Studies
Reproducibility of Research Conditions
In the realm of medical research, reproducibility is paramount. The lower extremity artery model provides a consistent and reliable platform for experimental studies. Unlike cadaveric specimens, which can vary significantly from one to another, these 3D-printed models offer a standardized baseline for research. This consistency allows researchers to conduct multiple trials under identical conditions, enhancing the validity and reliability of their findings. The ability to replicate exact anatomical conditions across different experiments is invaluable in comparative studies and in the development of new surgical techniques or medical devices.
Long-term Durability for Extended Research
The durability of these models is a significant advantage in long-term research projects. Unlike biological specimens that degrade over time, the silicone-based lower extremity artery models maintain their structural integrity and properties over extended periods. This longevity allows for prolonged studies, repeat experiments, and consistent training sessions without the need for frequent replacements. The models' resilience to repeated use makes them cost-effective for institutions conducting ongoing research or training programs, ensuring a stable and reliable research environment over time.
Standardization in Medical Education
In medical education, standardization is crucial for ensuring consistent learning outcomes. The lower extremity artery model provides a uniform learning experience for students and trainees across different institutions. This standardization is particularly valuable in assessing skills and knowledge, as it allows for fair comparisons and evaluations. Educational institutions can develop standardized curricula and assessment methods based on these models, ensuring that all students receive comparable training in vascular anatomy and interventional techniques. This uniformity in education contributes to maintaining high standards in medical training globally.
How Accurate Artery Models Improve Surgical Planning and Outcomes?
Enhanced Preoperative Visualization
The use of accurate lower extremity artery models significantly enhances preoperative planning. Surgeons can use these models to visualize complex anatomical structures in three dimensions, providing insights that 2D imaging alone cannot offer. This improved visualization allows for better strategizing of surgical approaches, particularly in cases involving intricate vascular networks or unusual anatomical variations. By handling a physical model that precisely replicates the patient's anatomy, surgeons can anticipate challenges, plan incision sites, and determine the most effective approach for procedures such as bypass grafting or endarterectomy. This level of preparation contributes to reduced surgical time and improved decision-making during the actual procedure.
Risk Mitigation in Complex Procedures
Accurate artery models play a crucial role in mitigating risks associated with complex vascular surgeries. By practicing on these models, surgeons can identify potential complications and develop strategies to address them before encountering them in the operating room. This is particularly valuable in high-risk procedures or when dealing with patients who have unusual anatomical structures. The ability to simulate various scenarios using these models allows surgical teams to prepare for contingencies, enhancing their readiness to handle unexpected situations during the actual surgery. This preparedness not only improves patient safety but also boosts the confidence of the surgical team, leading to more efficient and effective procedures.
Improved Patient Communication and Consent
The lower extremity artery model serves as an excellent tool for patient education and communication. Surgeons can use these models to explain complex procedures to patients and their families, providing a tangible representation of the planned intervention. This visual aid helps patients better understand their condition and the proposed treatment, facilitating informed decision-making and consent. The clarity provided by these models can alleviate patient anxiety by demystifying the surgical process. Moreover, this improved communication can lead to better patient compliance with pre- and post-operative instructions, contributing to improved overall outcomes and patient satisfaction.
Conclusion
The lower extremity artery model has revolutionized the field of vascular surgery and research, offering unprecedented accuracy and realism. Its anatomical precision, consistency in experimental studies, and ability to improve surgical planning and outcomes make it an invaluable tool for surgeons and researchers alike. As medical technology continues to advance, the role of such high-fidelity models in enhancing patient care, advancing medical research, and improving surgical outcomes cannot be overstated. The adoption of these models represents a significant step forward in the pursuit of excellence in vascular medicine and surgery.
Contact Us
At Trandomed, we are committed to advancing medical education and research through our state-of-the-art lower extremity artery models. As a leading supplier and manufacturer of 3D-printed medical simulators, we offer unparalleled quality and customization options to meet your specific needs. Experience the difference that accurate, reliable models can make in your surgical training or research. Contact us today at jackson.chen@trandomed.com to learn more about our products and how we can support your institution's goals in vascular medicine and surgery.