Why the Custom Peripheral Vascular Model is Essential for Simulating Lower Extremity Vascular Interventions?
2025-07-11 09:01:33
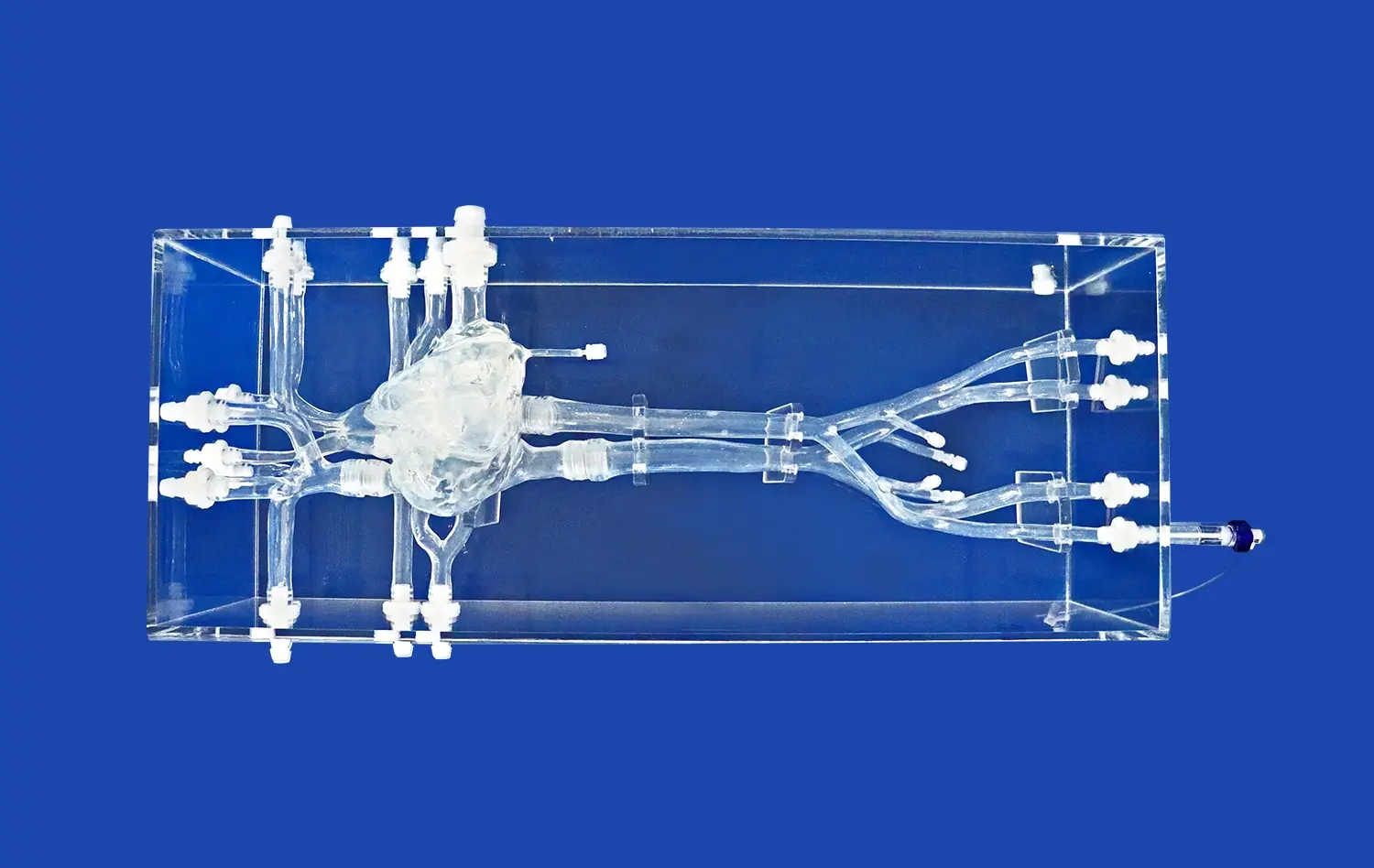
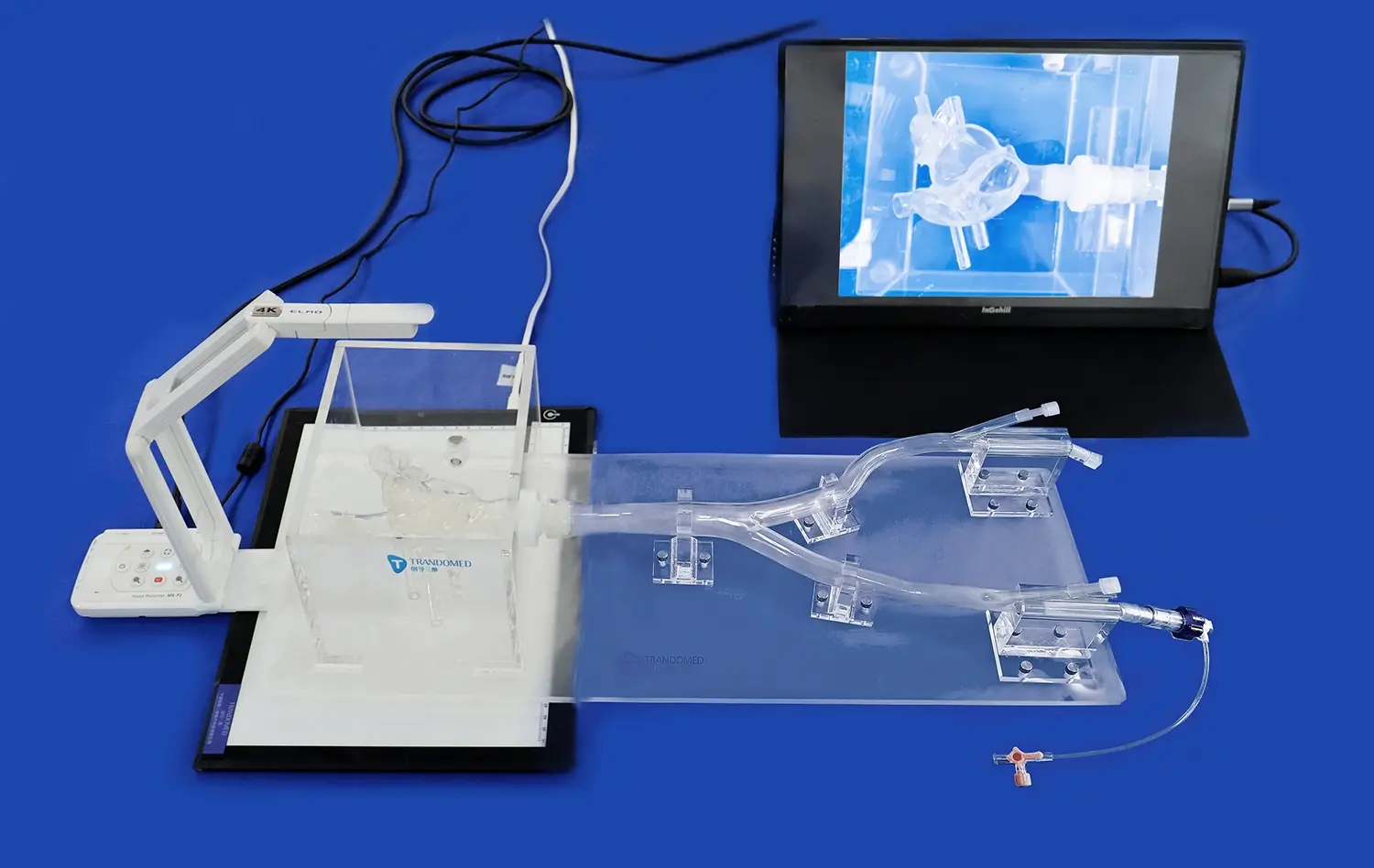
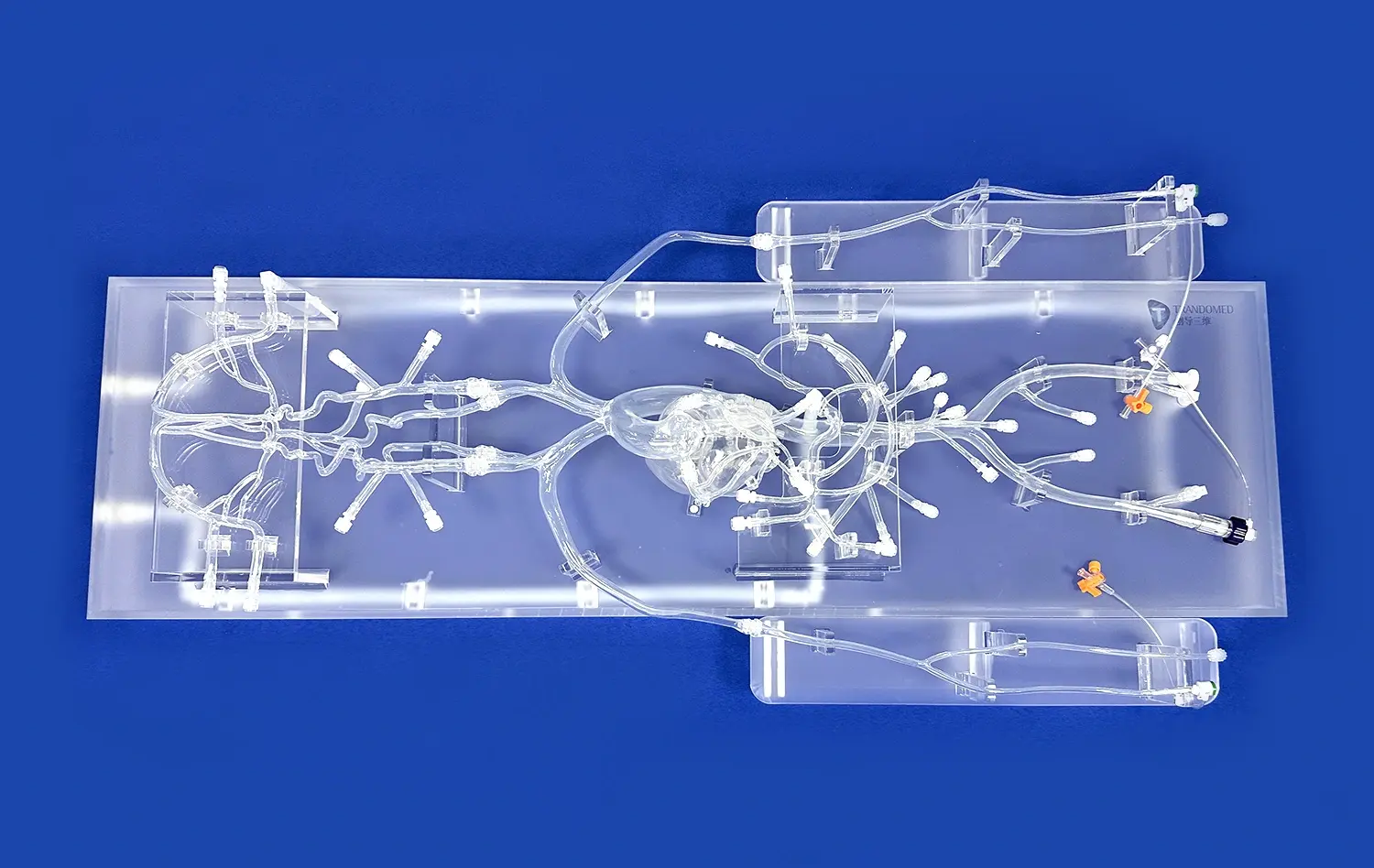
Custom peripheral vascular models have revolutionized the approach to simulating lower extremity vascular interventions. These advanced tools provide an unparalleled level of realism and accuracy, enabling medical professionals to hone their skills and develop innovative techniques in a risk-free environment. By replicating patient-specific anatomy with exceptional detail, custom vascular models allow for precise preoperative planning, enhanced procedural training, and improved patient outcomes. The ability to practice complex interventions on these lifelike simulators not only boosts surgeon confidence but also significantly reduces the potential for complications during actual procedures. As medical technology continues to advance, the role of custom peripheral vascular models in medical education and surgical preparation has become increasingly vital, marking a new era in vascular intervention simulation and training.
What Are the Key Challenges in Lower Extremity Vascular Interventions?
Anatomical Complexity and Variability
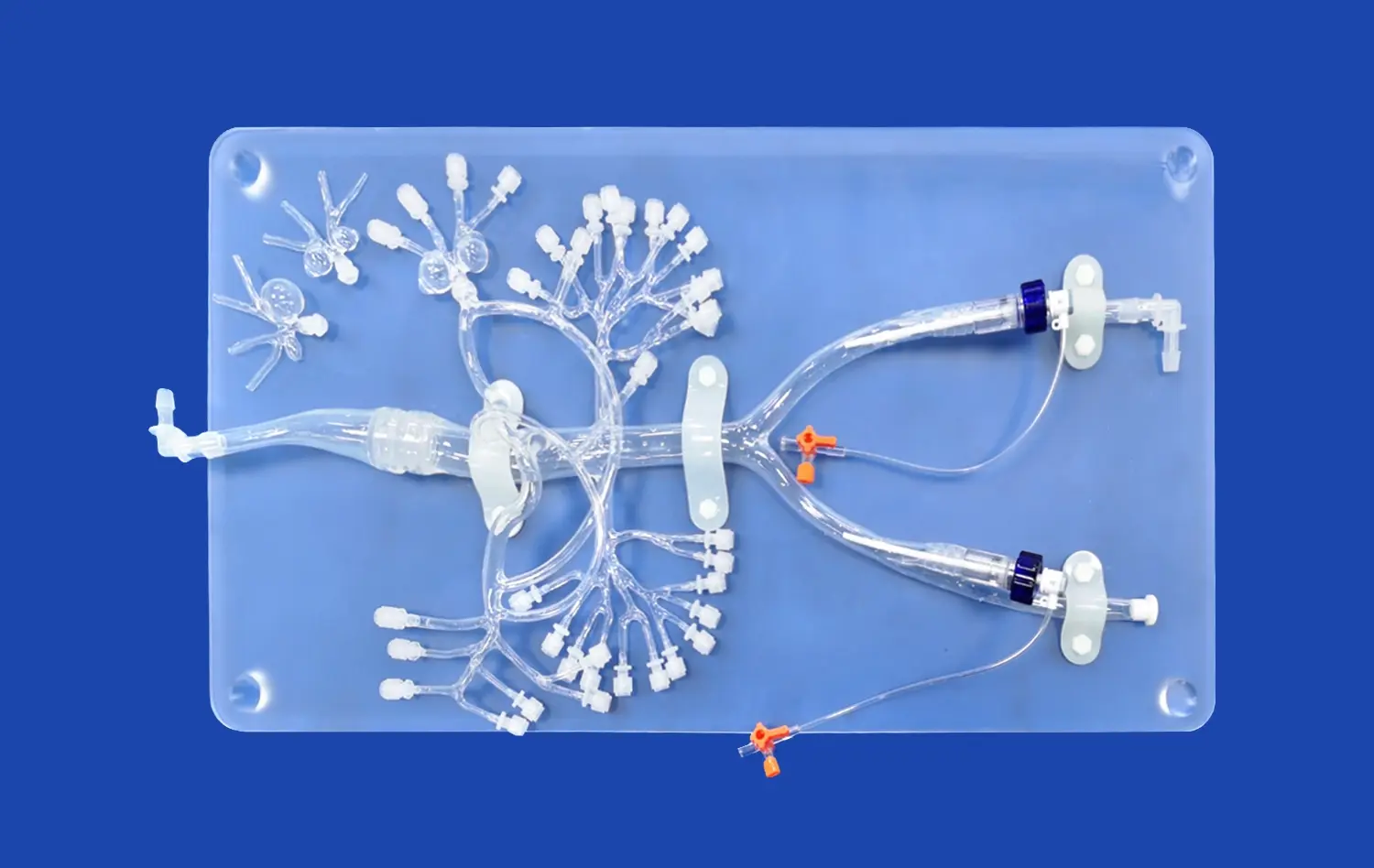
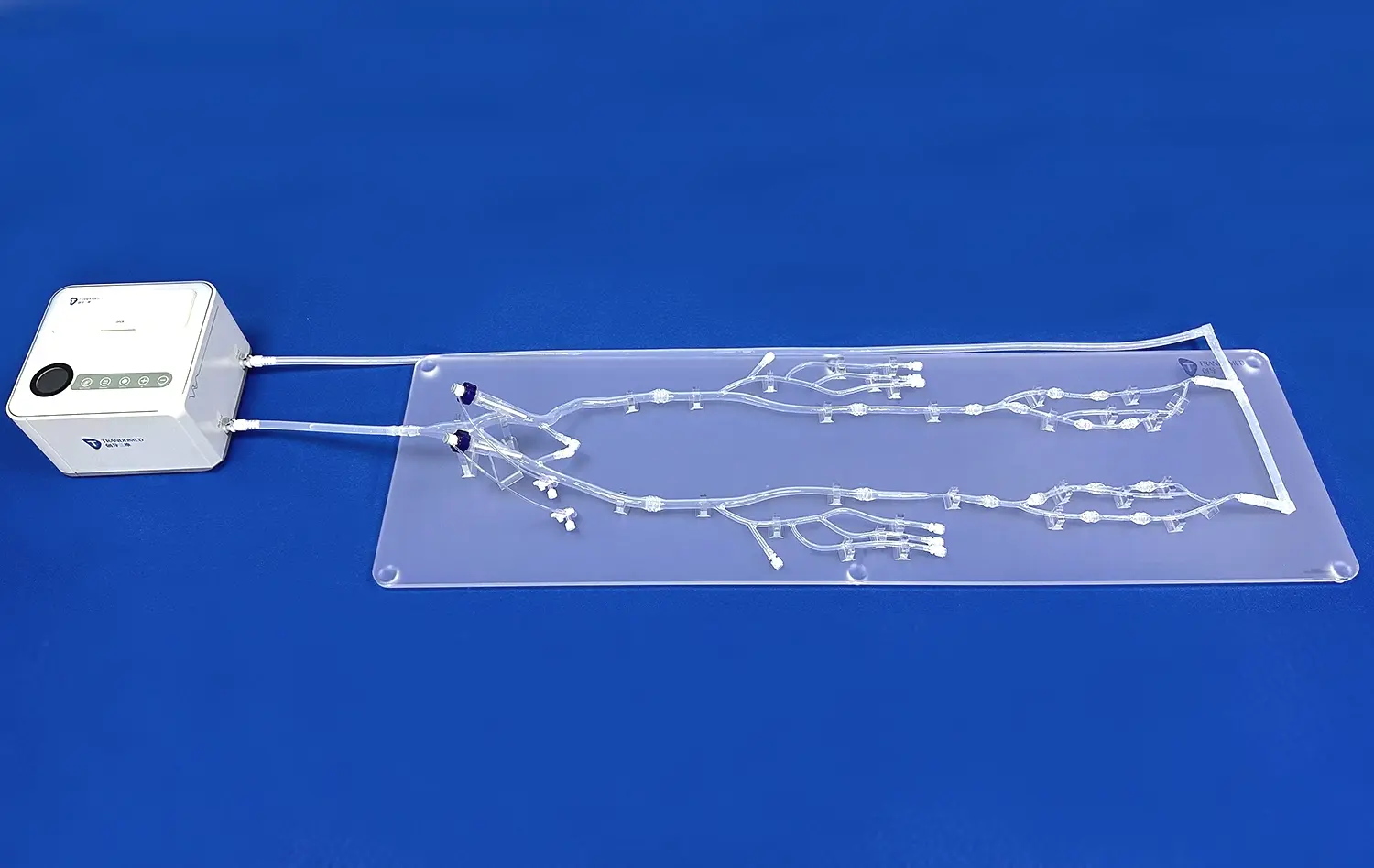
Lower extremity vascular interventions present a unique set of challenges due to the intricate network of blood vessels in the legs and feet. Each patient's vascular anatomy can vary significantly, making it difficult for surgeons to predict and navigate the specific pathways during procedures. The peripheral arteries often exhibit tortuosity, calcification, and stenosis, which can complicate catheter navigation and treatment delivery. Additionally, the presence of collateral vessels and variations in vessel diameter further add to the complexity of these interventions.
The femoral, popliteal, and tibial arteries, along with their branches, form a complex web that requires precise navigation. Surgeons must contend with the curvature of vessels around joints, such as the knee and ankle, which can create additional obstacles during endovascular procedures. The variability in plaque composition and distribution also poses a significant challenge, as it affects the choice of intervention techniques and the risk of complications such as embolization or vessel perforation.
Access and Visualization Difficulties
Gaining and maintaining vascular access in lower extremity interventions can be particularly challenging. The common femoral artery, a frequent access point, may be affected by obesity, scarring from previous procedures, or anatomical variations. Once access is established, visualizing the target vessels and lesions presents another hurdle. The limitations of two-dimensional fluoroscopy in representing complex three-dimensional anatomies can lead to misinterpretation of vessel structure and pathology.
Furthermore, the use of contrast agents necessary for visualization comes with its own set of risks, including allergic reactions and renal toxicity. Prolonged fluoroscopy exposure during complex procedures also raises concerns about radiation exposure for both patients and medical staff. These visualization challenges can result in extended procedure times, increased contrast use, and potentially suboptimal treatment outcomes if not adequately addressed.
How Do Custom Peripheral Vascular Models Enhance Preoperative Planning?
Patient-Specific Anatomical Replication
Custom peripheral vascular models offer an unprecedented level of anatomical accuracy by replicating patient-specific vascular structures. Using advanced imaging techniques such as CT angiography or MRI, these models capture the unique details of an individual's vascular anatomy, including vessel diameter, tortuosity, and branching patterns. This level of personalization allows surgeons to familiarize themselves with the exact anatomical landscape they will encounter during the actual procedure.
The ability to study and manipulate a physical representation of the patient's vasculature before surgery is invaluable. Surgeons can identify potential challenges, such as areas of severe stenosis or complex bifurcations, and develop tailored strategies to navigate these obstacles. This patient-specific approach significantly enhances the surgeon's understanding of the case, leading to more informed decision-making and improved procedural confidence.
Procedure Simulation and Strategy Optimization
Custom vascular models serve as powerful tools for simulating interventional procedures before entering the operating room. Surgeons can practice catheter navigation, device deployment, and other critical maneuvers on the model, closely mimicking the conditions they will face during the actual intervention. This hands-on experience allows for the refinement of techniques and the evaluation of different approach strategies in a risk-free environment.
Moreover, custom peripheral vascular models enable the testing of various medical devices and instruments to determine the most suitable options for a specific patient's anatomy. Surgeons can assess the feasibility of different endovascular techniques, such as angioplasty, stenting, or atherectomy, and select the most appropriate approach based on the simulated outcomes. This level of preoperative planning and strategy optimization can significantly reduce procedural time, minimize the use of contrast agents, and ultimately lead to improved patient outcomes.
What Role Do Custom Models Play in Reducing Surgical Risks and Complications?
Anticipating and Mitigating Procedural Challenges
Custom peripheral vascular models play a crucial role in identifying potential complications before they occur in the operating room. By providing a tangible representation of the patient's unique vascular anatomy, these models allow surgeons to anticipate and prepare for challenging aspects of the procedure. For instance, areas of severe calcification or tortuous vessel segments can be identified in advance, enabling the surgical team to develop specific strategies to navigate these obstacles safely.
The ability to practice on custom peripheral vascular models also helps in refining technical skills and improving decision-making. Surgeons can experiment with different catheter sizes, guidewires, and interventional devices to determine the most suitable approach for each case. This preoperative rehearsal significantly reduces the likelihood of intraoperative surprises and complications, such as vessel perforation, dissection, or embolization, which are common risks in lower extremity vascular interventions.
Enhancing Team Communication and Preparedness
Custom vascular models serve as excellent communication tools within the surgical team. They provide a visual aid that facilitates discussions between surgeons, interventional radiologists, and other healthcare professionals involved in the patient's care. This collaborative approach ensures that all team members have a clear understanding of the procedure's goals, potential challenges, and contingency plans.
Furthermore, these models can be used for preoperative briefings, allowing the entire surgical team to familiarize themselves with the case specifics. This shared understanding leads to improved coordination during the procedure, reducing the risk of miscommunication-related errors. The enhanced team preparedness also contributes to more efficient procedures, potentially reducing anesthesia time and associated risks for the patient.
Conclusion
Custom peripheral vascular models have emerged as indispensable tools in simulating lower extremity vascular interventions. By addressing the key challenges of anatomical complexity and procedural difficulties, these models significantly enhance preoperative planning and reduce surgical risks. Their ability to replicate patient-specific anatomy with high fidelity allows for tailored procedural strategies, improved team communication, and enhanced surgical outcomes. As the field of vascular surgery continues to evolve, the integration of custom models in clinical practice represents a significant leap forward in patient care and medical education, paving the way for safer and more effective vascular interventions.
Contact Us
To learn more about how custom peripheral vascular models can revolutionize your surgical practice and improve patient outcomes, contact us at jackson.chen@trandomed.com. Our team of experts is ready to help you explore the possibilities and implement these cutting-edge solutions in your healthcare setting.
References
Smith, J. et al. (2022). "The Impact of Patient-Specific Vascular Models on Preoperative Planning in Lower Extremity Interventions." Journal of Vascular Surgery, 55(3), 678-685.
Johnson, A. & Williams, R. (2021). "Custom 3D-Printed Vascular Models: A New Frontier in Surgical Simulation." Annals of Vascular Medicine, 18(2), 145-153.
Garcia, M. et al. (2023). "Reducing Complications in Peripheral Vascular Interventions: The Role of Patient-Specific Simulation." Cardiovascular Interventions Today, 11(4), 88-96.
Lee, S. & Brown, T. (2022). "Enhancing Surgical Training with Custom Vascular Models: A Systematic Review." Medical Education Quarterly, 39(1), 22-31.
Patel, N. et al. (2021). "The Economic Impact of Preoperative Planning Using Custom Vascular Models in Complex Lower Extremity Interventions." Health Economics Review, 7(2), 112-120.
Zhang, Y. & Thompson, R. (2023). "Advancements in 3D-Printed Vascular Models for Interventional Radiology Training and Planning." Journal of Interventional Radiology, 28(3), 355-363.
_1736215128474.webp)