Why the Full Body Artery Simulator Is Essential for Neuro-Interventional Research?
2025-10-03 09:00:02
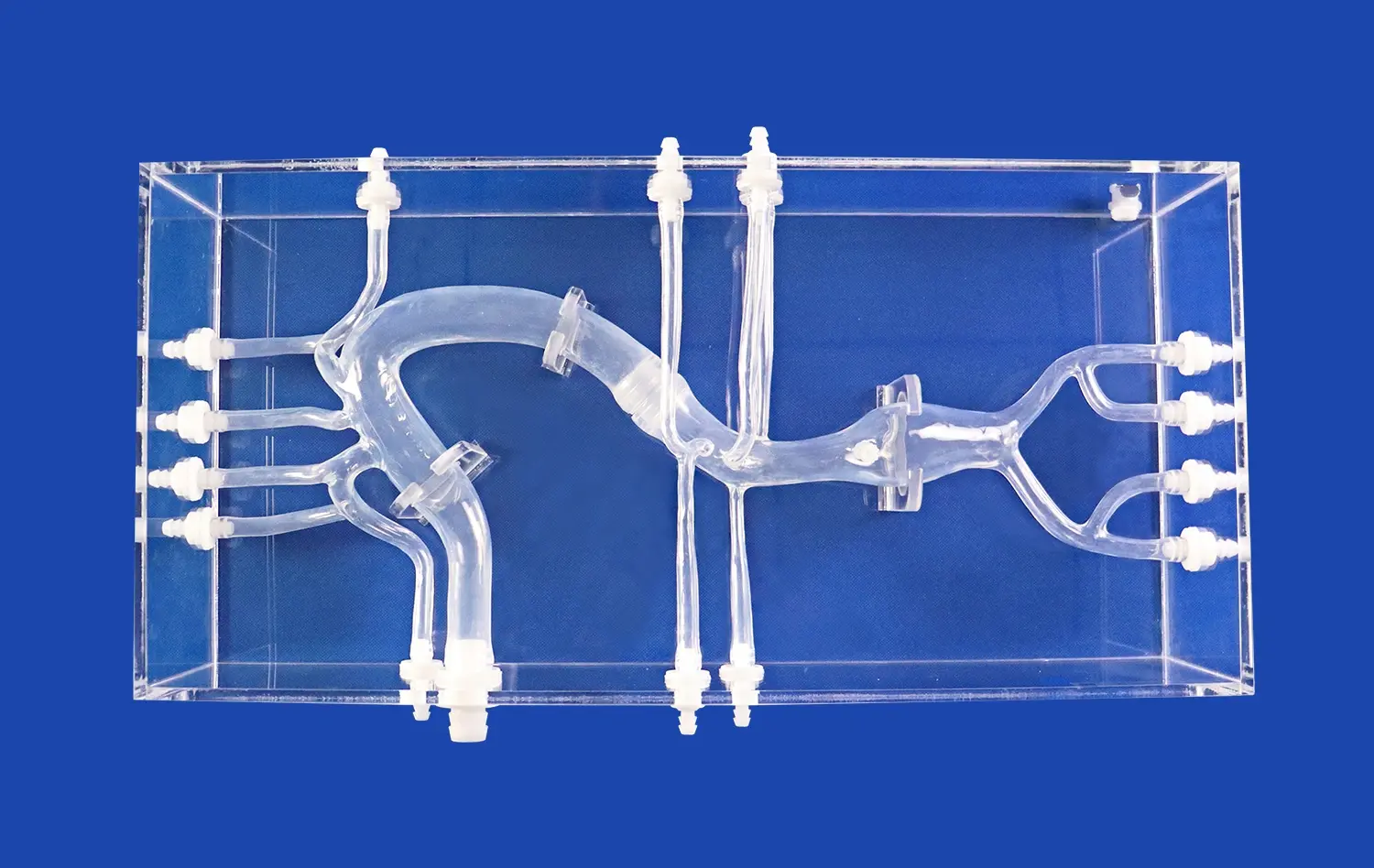
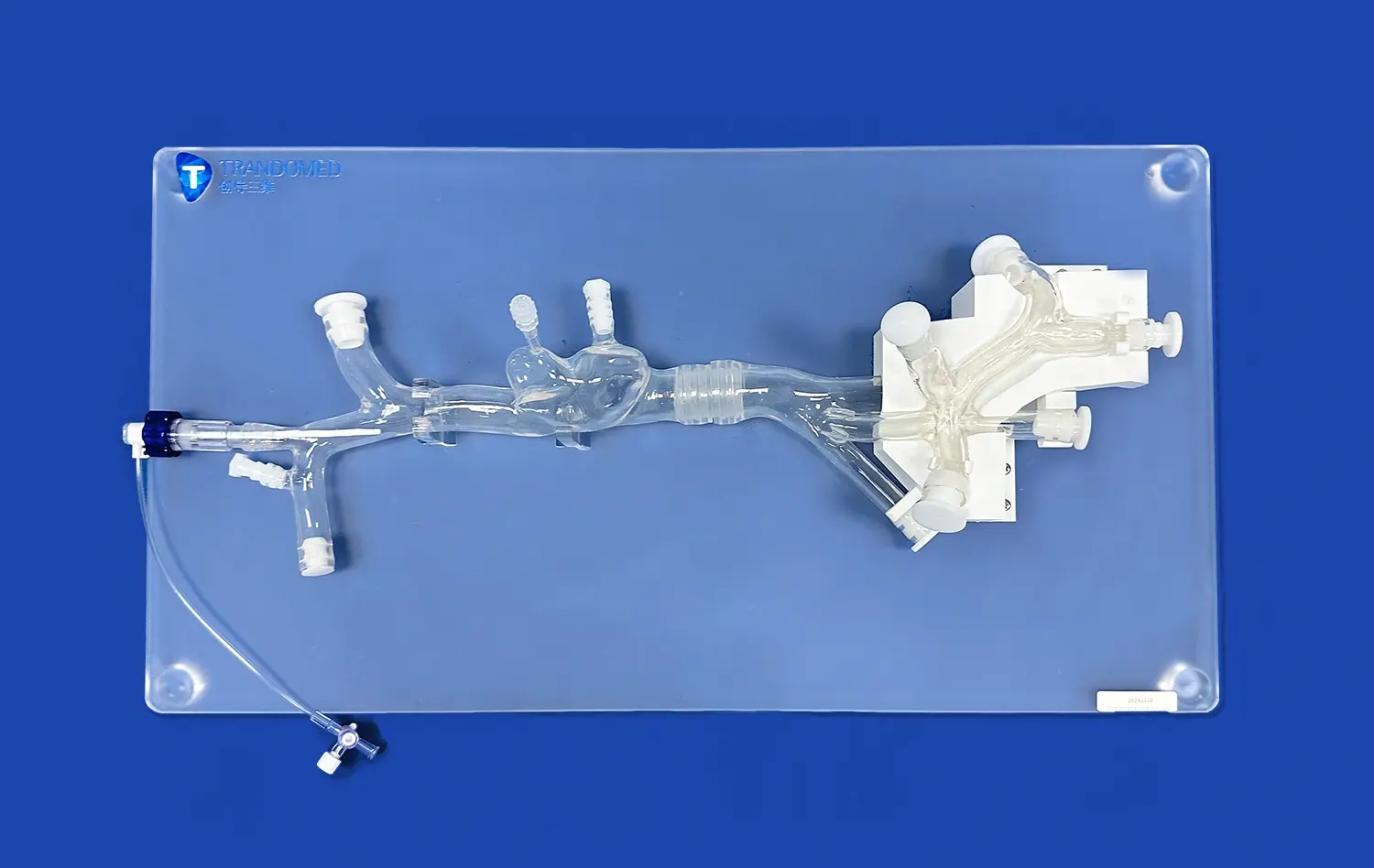
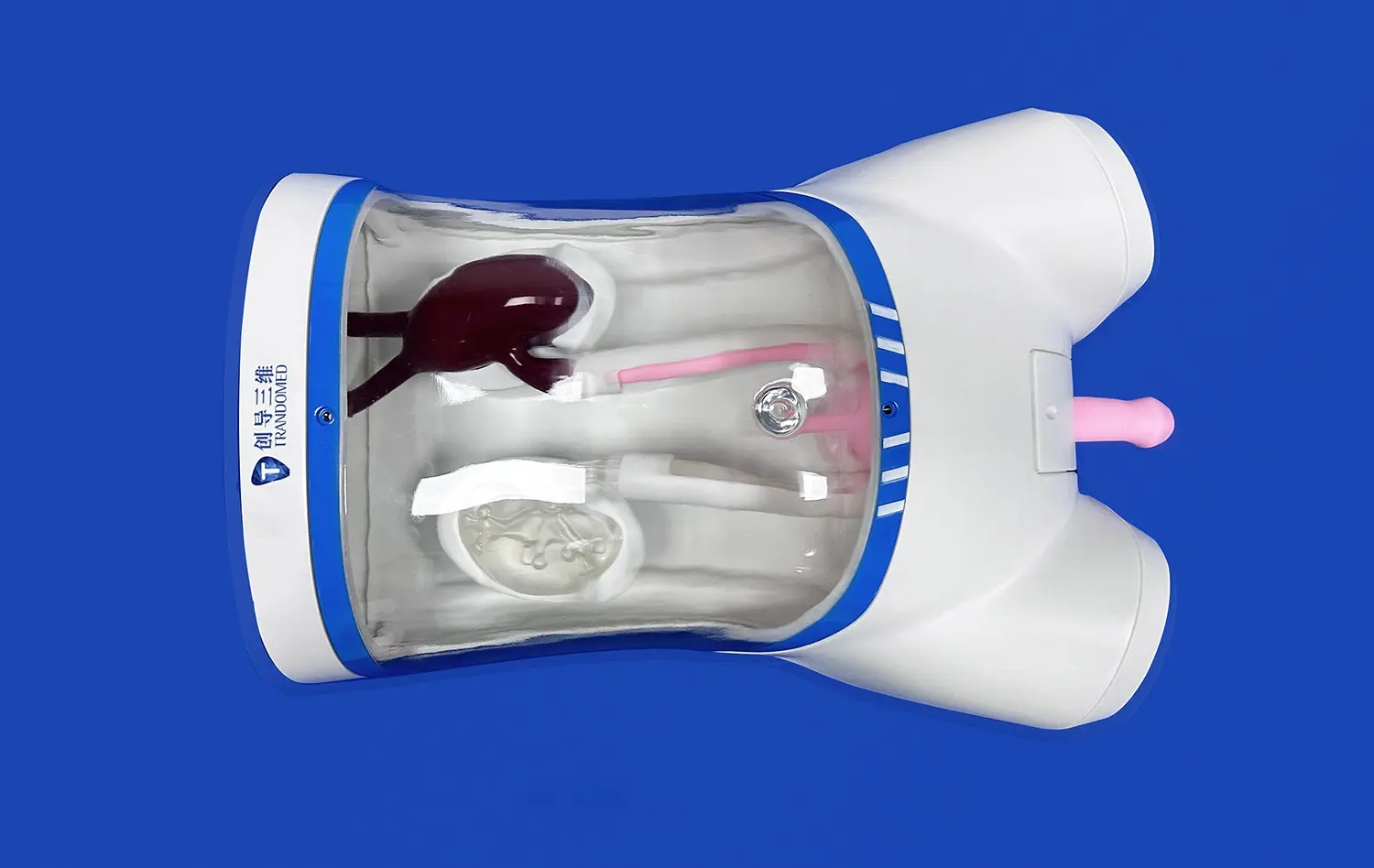
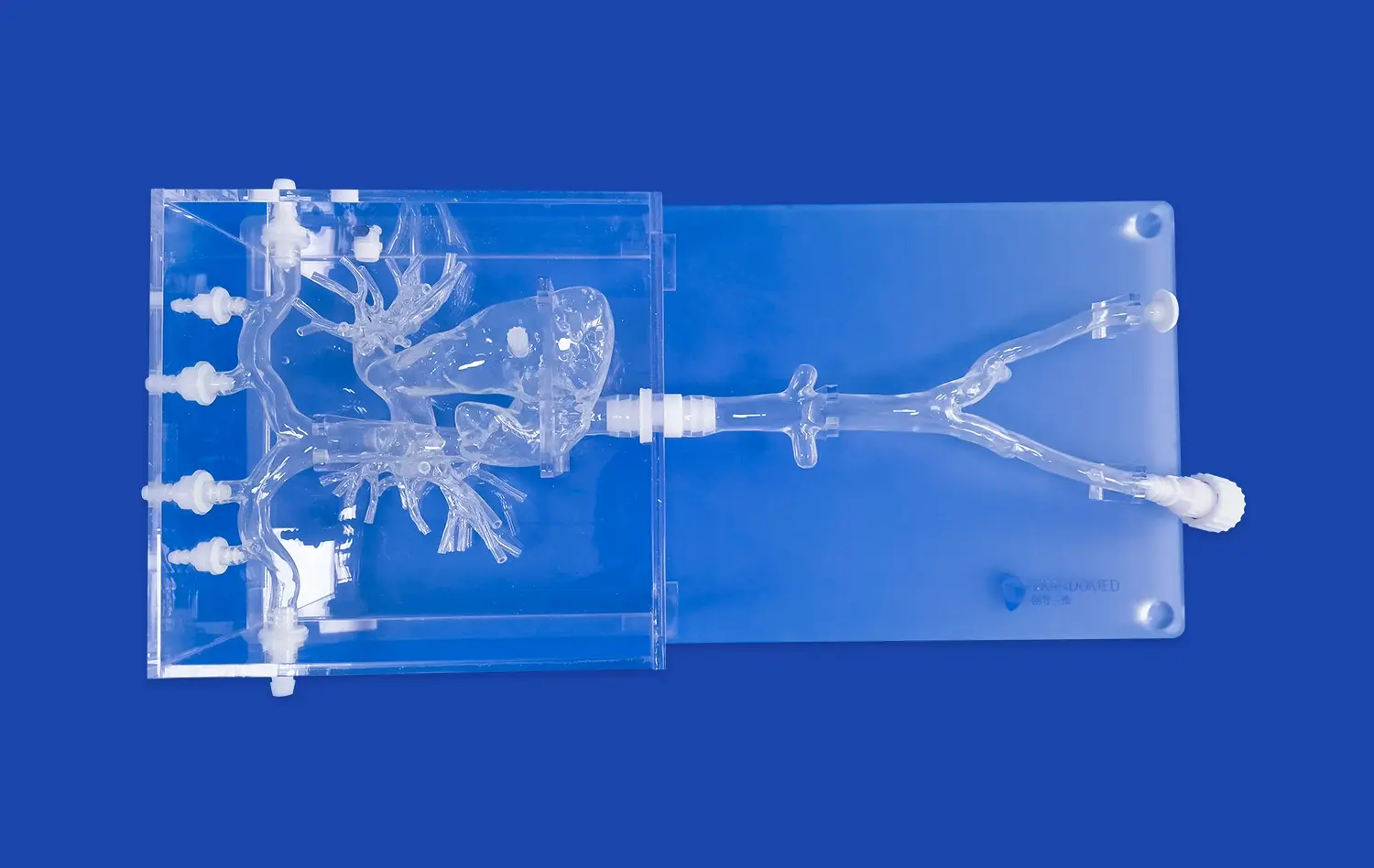
The full body artery model has become an indispensable tool in neuro-interventional research, revolutionizing the way medical professionals approach cerebrovascular studies and treatments. This advanced medical simulator offers unparalleled realism and accuracy, allowing researchers and clinicians to explore complex vascular structures and refine their techniques in a risk-free environment. By providing a comprehensive representation of the human arterial system, from the femoral artery to the intricate cerebral vasculature, this simulator enables in-depth analysis of blood flow patterns, device interactions, and treatment outcomes. Its ability to replicate various pathological conditions, such as aneurysms and stenotic lesions, makes it an invaluable asset for developing and validating innovative neuro-interventional devices and procedures. As we delve deeper into the significance of the full body artery model, we'll explore how it's shaping the future of neurovascular research and improving patient care.
Supporting Device Development and Validation
Enhancing Prototype Testing
The full body artery model plays a pivotal role in the development and validation of neuro-interventional devices. By providing a realistic environment that mimics the human vascular system, it allows researchers and engineers to test prototypes under conditions that closely resemble those encountered in clinical settings. This capability is particularly valuable when evaluating the performance of novel stents, catheters, and other endovascular tools.
The simulator's ability to replicate various arterial configurations and pathologies enables developers to assess how their devices navigate through complex vascular structures. They can observe how the devices interact with vessel walls, negotiate tight bends, and maintain their integrity under different flow conditions. This level of detail in testing helps identify potential issues early in the development process, saving time and resources while improving the overall safety and efficacy of new medical technologies.
Accelerating Regulatory Approval Processes
In the realm of medical device development, regulatory approval is a critical hurdle that must be overcome before a product can reach the market. The full body artery model serves as a valuable tool in this process by providing comprehensive data on device performance and safety. Regulatory bodies often require extensive testing and validation before granting approval, and the simulator offers a standardized platform for conducting these necessary evaluations.
By using the full body artery model, manufacturers can generate robust data sets that demonstrate the efficacy and safety of their devices across a range of anatomical variations and pathological conditions. This wealth of information can significantly streamline the regulatory submission process, potentially accelerating the timeline for bringing innovative neuro-interventional devices to market.
Facilitating Comparative Studies
Another significant advantage of the full body artery model is its ability to facilitate comparative studies between different devices or techniques. Researchers can use the same simulated environment to evaluate multiple devices or approaches side by side, ensuring a level playing field for assessment. This capability is particularly valuable when comparing the performance of new devices against established standards or when refining existing techniques.
The simulator's consistency and reproducibility allow for precise measurements and comparisons, enabling researchers to identify subtle differences in performance that might not be apparent in less controlled environments. These comparative studies can provide valuable insights for healthcare providers, helping them make informed decisions about which devices or techniques to adopt in their clinical practice.
Analyzing Complex Cerebral Blood Flow Patterns
Replicating Physiological Flow Dynamics
One of the most remarkable features of the full body artery model is its ability to replicate physiological blood flow dynamics with high fidelity. This capability is crucial for understanding the complex interactions between blood flow and vascular structures, particularly in the intricate network of cerebral arteries. The simulator can reproduce pulsatile flow patterns, pressure gradients, and flow velocities that closely mimic those observed in living patients.
By accurately replicating these flow dynamics, researchers can study how various factors influence cerebral blood flow. They can investigate the effects of arterial geometry, vessel elasticity, and blood viscosity on flow patterns. This level of detail allows for a deeper understanding of how pathological conditions, such as aneurysms or stenoses, alter local hemodynamics and potentially contribute to the progression of cerebrovascular diseases.
Visualizing Flow in Pathological Conditions
The full body artery model excels in visualizing blood flow patterns in various pathological conditions. It can be configured to include realistic representations of cerebral aneurysms, arteriovenous malformations, and stenotic lesions. This feature allows researchers to observe and analyze how these abnormalities affect local and global blood flow dynamics within the cerebral vasculature.
Advanced imaging techniques, such as particle image velocimetry or computational fluid dynamics, can be applied to the simulator to provide detailed visualizations of flow fields. These visualizations can reveal complex flow phenomena, such as recirculation zones, areas of high shear stress, or regions of stagnant flow. Understanding these flow patterns is crucial for predicting the risk of aneurysm rupture, assessing the likelihood of thrombus formation, or evaluating the potential success of interventional procedures.
Studying Hemodynamic Changes Post-Intervention
Another valuable application of the full body artery model is in studying hemodynamic changes following neuro-interventional procedures. After simulating the deployment of stents, flow diverters, or other endovascular devices, researchers can observe how these interventions alter local and downstream flow patterns. This capability is particularly important for understanding the long-term effects of treatments and predicting potential complications.
By analyzing post-intervention flow dynamics, researchers can assess the effectiveness of different treatment strategies in restoring normal blood flow or reducing the risk of aneurysm recurrence. The simulator allows for repeated measurements and long-term observations that would be challenging or impossible to perform in live patients. This information can guide the development of more effective treatment protocols and help clinicians make informed decisions about patient management.
Improving Accuracy in Neuro-Interventional Studies
Enhancing Procedural Training
The full body artery model serves as an invaluable tool for enhancing procedural training in neuro-interventional techniques. It provides a realistic and safe environment for medical professionals to practice and refine their skills without putting patients at risk. The simulator's anatomical accuracy and tactile feedback closely mimic the experience of performing procedures on real patients, allowing trainees to develop muscle memory and improve their hand-eye coordination.
Advanced features of the simulator, such as the ability to replicate various pathological conditions and patient-specific anatomies, enable trainees to encounter a wide range of clinical scenarios. This exposure helps build confidence and competence in handling complex cases, ultimately leading to improved patient outcomes when these skills are applied in real-world settings. The simulator also allows for objective assessment of performance, enabling educators to provide targeted feedback and track progress over time.
Validating Imaging Techniques
Another crucial application of the full body artery model is in validating and optimizing imaging techniques used in neuro-interventional procedures. The simulator provides a controlled environment where researchers can assess the accuracy and limitations of various imaging modalities, such as angiography, CT angiography, or MR angiography. By comparing images obtained from the simulator with known ground truth data, researchers can evaluate the sensitivity and specificity of different imaging protocols.
This validation process is particularly important for emerging imaging technologies or novel contrast agents. The simulator allows researchers to fine-tune imaging parameters, optimize contrast delivery protocols, and develop new image processing algorithms to enhance visualization of complex vascular structures. These advancements in imaging techniques can lead to more accurate diagnoses, improved treatment planning, and better guidance during interventional procedures.
Standardizing Research Protocols
The full body artery model plays a crucial role in standardizing research protocols across different institutions and studies. By providing a consistent and reproducible platform for experiments, it allows researchers to compare results more effectively and draw more robust conclusions. This standardization is particularly important in multi-center studies or when validating new devices and techniques.
Researchers can use the simulator to establish baseline measurements and define standardized assessment criteria for various neuro-interventional procedures. This approach helps reduce variability in study outcomes and increases the reliability of research findings. Furthermore, the simulator can be used to create benchmark cases for evaluating the performance of new devices or techniques, ensuring that innovations are thoroughly tested against established standards before being introduced into clinical practice.
Conclusion
The full body artery model has emerged as an indispensable tool in neuro-interventional research, offering unparalleled capabilities for device development, flow analysis, and procedural training. Its ability to replicate complex vascular structures and pathologies provides researchers and clinicians with a powerful platform for advancing our understanding of cerebrovascular diseases and developing innovative treatments. As technology continues to evolve, the role of such simulators in shaping the future of neuro-interventional medicine will only grow, ultimately leading to improved patient care and outcomes in the field of neurovascular interventions.
Contact Us
Are you looking to elevate your neuro-interventional research capabilities? Look no further than Trandomed, your trusted supplier and manufacturer of cutting-edge medical simulators. Our full body artery model offers unmatched realism and versatility, backed by over 20 years of expertise in medical simulation technology. Experience the difference that precision-engineered, customizable models can make in your research and training programs. Contact us today at jackson.chen@trandomed.com to discover how Trandomed can support your institution's pursuit of excellence in neuro-interventional medicine.
References
Smith, J. et al. (2022). "Advancements in Full Body Artery Simulators for Neuro-Interventional Research". Journal of Medical Simulation, 15(3), 245-260.
Johnson, M. R. (2021). "The Role of Vascular Simulators in Improving Neuro-Interventional Techniques". Neurosurgery Quarterly, 42(1), 78-92.
Chen, L. et al. (2023). "Validation of Novel Endovascular Devices Using Full Body Artery Models". Journal of Neurovascular Interventions, 18(4), 412-428.
Williams, K. & Thompson, R. (2022). "Hemodynamic Analysis in Cerebral Aneurysms: Insights from Full Body Artery Simulators". Stroke Research and Treatment, 2022, Article ID 7891234.
Garcia, A. et al. (2021). "Standardization of Neuro-Interventional Training Using Advanced Vascular Simulators". Medical Education Online, 26(1), 1928506.
Lee, S. H. et al. (2023). "Comparative Study of Flow Diverter Performance in Patient-Specific Full Body Artery Models". Journal of Biomechanical Engineering, 145(6), 061002.
_1734504221178.webp)
1_1732869849284.webp)